Meniscal repairs: A review of past, current, and future options
Mr Kamil Wegrecki, A/Prof. Nigel Hope, Dr Danè Dabirrahmani, Dr Andrew Stuart
Wednesday, September 21st, 2016
Meniscal tears are amongst the most common knee injuries. The purpose of the current article is to identify the most common meniscal tears, current treatment options, and potential future treatment methods. The traditional approach to meniscal tears was total meniscectomy. However, this approach has been largely abandoned due to the emergent relationship between even partial meniscectomy and the early onset and development of osteoarthritis. Complete meniscectomy is indicated only if the meniscus is torn beyond repair, however, preservation of the meniscal rim is always a priority. Tears in the peripheral one-third region are well suited for repair and these have high success rates. When irreparable damage is encountered, removal and replacement of the meniscus with natural or synthetic scaffolds presents a promising option if its efficacy can be definitively demonstrated in future trials.
Introduction
The menisci are a pair of semilunar, wedge-shaped fibrocartilaginous structures sitting between the femur and the tibia within the tibiofemoral joint of each knee. They are involved in load transmission and produce significant load-spreading across the articular surfaces in normal knees [1,2], as well as shock-absorption, which is reduced in painful knees [3]. Other meniscal functions include joint lubrication [4], structural stability [5], and proprioception [6].
Meniscal tears are among the most common knee injuries and can be secondary to trauma or degenerative changes [7]. The former occurs when excessive force is applied to a normal meniscus while the latter occurs from normal forces acting on a degenerative structure [8]. Acute tears are usually caused by a traumatic, twisting motion of the knee, frequently during sports [7]. Sports-related meniscal tears are often associated with anterior cruciate ligament (ACL) rupture [7,9].
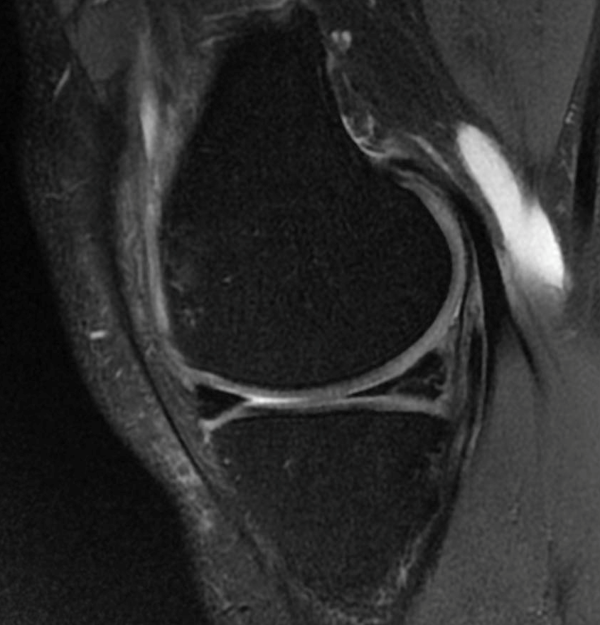
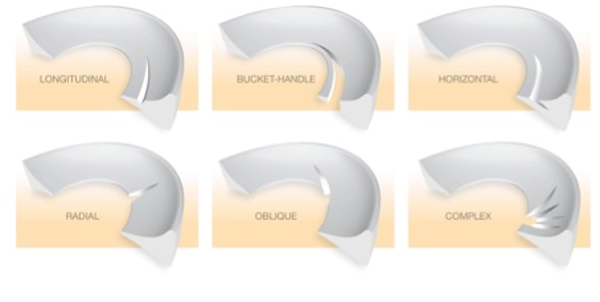
In addition to the two aetiological categories mentioned, meniscal tears can be classified according to the pattern of rupture seen at arthroscopy [8]. The most commonly described patterns of meniscal injury are as follows:
- Horizontal (cleavage) tears: These tears result from shear stresses generated by inferior and superior sections of the meniscus, causing the meniscus to cleave into two layers [7,8]. Horizontal tears are difficult to manage and are not usually amenable to repair.
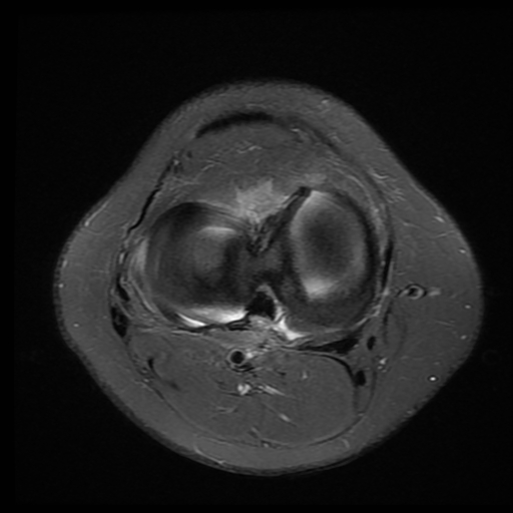
- Vertical (longitudinal/circumferential) tears (Figure 1): These are the most common type of meniscal tear to be repaired. They can vary in size between ~1mm to the full length of the meniscus [8]. The Bucket-handle tear (Figure 2) is a type of vertical longitudinal tear in which the inner margin is displaced from the remainder of the meniscus. Depending on the extent of injury, it can be unstable and cause mechanical symptoms such as the classical “lock knee” [8]. Owing to its more secure attachment to the tibial plateau, the medial meniscus is more prone to shear forces and is more commonly affected [8].
Figure 1: Peripheral longitudinal tear. Source: Dr Andrew Stuart
Figure 2: Bucket-handle tear. Source: Dr Andrew Stuart
- Oblique (flap/parrot-beak) tears (Figure 3): These are tears that proceed towards the periphery at an acute angle to the meniscal margin. Oblique tears can occur at any point along the meniscus but most often between the posterior- and middle-thirds of the meniscus. Propagation of the tear or mechanical symptoms can be elicited by a free flap catching in the articular interface [8]. Along with vertical tears, they make up 81% of all tears [8].
Figure 3: Oblique (flap) tear. Source: Dr Andrew Stuart
- Radial (transverse) tears: These are tears that occur across the circumferential fibers of the meniscus (Figure 4). They are commonly seen following ACL disruption. Radial tears may extend to the periphery if not treated, at which point they disrupt the natural hoop stresses of the meniscus and interfere with its natural load-spreading and shock-absorptive functions [8].
Figure 4: Types of meniscal tears. Source: Hope Orthopaedics
- Complex tears: These are degenerative in nature, composed of several different tears in multiple planes resulting from persistent hoop and sheer stresses, and are often associated with degeneration of articular cartilage [10]. Together, they feature in the pathology of degenerative arthritis, which is positively associated with older age [8,11]. The healing potential of chronic degenerative menisci remains poor and conservative treatment is recommended except in refractory cases [10].
Methods
A literature search of publications relating to meniscal repairs was undertaken. The databases PubMed, CINAHL, and Ovid were searched. The search terms “Meniscus OR Meniscal”, “Tear”, “Treatment OR Repair OR Surgery”, “Knee”, “Options” and “Outcome” were used. This search yielded 453 publications. Additional articles were obtained from bibliographic screening. After the search, articles that were not relevant to meniscal tears of the knee and treatment options were excluded. In the final analysis, 37 articles were included in the current review.
Meniscectomy
The traditional approach to meniscal tears, until the 1970s, was total meniscectomy [11]. However, this approach has been largely abandoned due to the emergent relationship between even partial meniscectomy and the early onset and development of osteoarthritis (OA) [7,12-15]. Meniscectomies have been shown to cause joint-space narrowing, lowering the rate of regeneration, leading to an increase in the degenerative changes in the surrounding cartilage, and hence a higher incidence of OA [16-20]. In a normal knee, the menisci transmit 50% of joint-compressive forces in full extension and 85% of the load at 90° of flexion [21]. However, following a total meniscectomy, the tibiofemoral contact area is reduced by approximately 75%, while contact forces increase by 235% [1,2]. Today, repair and preservation of the menisci is the universally-accepted approach to meniscal tears.
Untreated meniscal damage is a potent risk factor for the development of OA [22]. When meniscal repair is not possible, partial meniscal resection is preferred to total meniscectomy, and is associated with less radiographic OA over time [22,23]. A systematic review of clinical outcomes found lateral meniscectomy to be associated with significantly greater frequency of radiographic OA, reduced knee function and future instability than medial meniscectomy [24]. The lateral meniscus has been reported to carry a higher load in the knee compared with the medial meniscus, and its loss may result in increased cartilage contact stress [22]. Furthermore, degenerative meniscal tear and cartilage changes at the time of surgery were associated with radiographic OA more frequently than were longitudinal tear and absence of cartilage changes, respectively [22].
Current treatment methods
Meniscus surgery procedures have rapidly developed from open procedures to arthroscopic surgery over the past two decades [25]. Reparability of the meniscus depends on several factors, such as vascularity, type of tear, chronicity, and size [15,26]. Complete meniscectomy is indicated only if the meniscus is torn beyond repair, however, preservation of the meniscal rim is always a priority [15,26,27].
The indications for meniscus repair include: active patients with tibiofemoral joint line pain, patients younger than 50, or patients between 50 and 60 who are athletically active. Repair may also be undertaken with concurrent knee-ligament reconstruction, a reducible meniscus tear, and good tissue integrity [28].
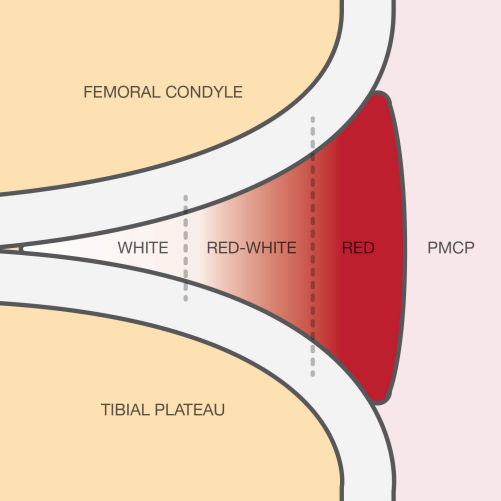
Tears in the peripheral one-third region (zone 1, also known as the red-red zone due to its high vascularity; Figure 5) are well suited for repair, and these have high success rates. Tears in the middle-third region (zone 2, also known as the red-white zone) are often reparable with reasonable success rates. Longitudinal, radial, and horizontal tears confined to zones 1 and 2 are patterns that are usually amenable to repair [28-30]. The vascularity of the menisci is important, as it is critical to the success of a healing response. Meniscal vascularity has been described by Arnoczky and Warren [31]. The degree of vascular penetration was found to be 10-30% of the width of the medial meniscus, and 10-25% of the width of the lateral meniscus. Therefore, tears in the vascular zone have the highest chance of healing. Cannon and Vittori [32] reported a decline in healing rates as tear location moved from peripheral to central: 90% for tears within 2 mm of the periphery, 74% for tears within 3 mm of the periphery and 50% for tears within 4-5 mm of the periphery. The length of the tear has also been suggested to affect repair outcome. Cannon and Vittori [32] reported 90% and 50% healing rates for tears less than 2 cm and greater than 4 cm, respectively. Bach et al. [33] documented significantly earlier failure in larger tears. However, other data has been unable to demonstrate a significant difference in repair outcomes based on tear length [33].
Figure 5: Types of meniscal tears. Source: Hope Orthopaedics
The identification of meniscal tears suitable for repair is usually made at the time of arthroscopy. The three general meniscal repair techniques are as follows:
- Inside-out repair technique: This technique uses sutures placed in the menisci from within the joint cavity and tied over the capsule through a limited open approach. This technique is the gold standard with which other repair techniques are compared [34,35]. However, comparable results are reported with other techniques that are less technically demanding [35].
- Outside-in repair technique: Sutures are introduced into the knee through the lumen of a standard spinal needle, where they are visualised by the arthroscope. The suture is then drawn through a portal and interference knot tied. The knot is pulled back into the knee where it tamps down the torn meniscal fragments. This technique is mostly suited to tears in the anterior and adjacent middle segments of the meniscus [36].
- All-inside repair technique: This is a more recent technique, favoured by most clinicians due to its lower complication rate and lower morbidity [37,38]. It can be divided into two types: one that uses resorbable, rigid arrows (darts and staples), which provide rigid fixation, and one that employs flexible, suture-based repair devices, which deploy anchors for stability [39]. These arrows and sutures are designed to hold the meniscal fragments together while healing occurs. They are popular, as they do not necessitate an additional skin incision. However, some of the rigid devices have demonstrated inferior mechanical properties compared with sutures [39-41]. Suture-based devices were developed in an attempt to avoid the complications associated with rigid devices and to allow a more flexible fixation of the meniscal fragments [42]. Success rates of 83-88% have been reported for this technique [43,44].
Arthroscopic trephination of vascular channels at the free meniscal edges has also shown improved meniscal healing. Trephination is a safe and easy procedure that involves the creation of a channel through the meniscus from the vascularised zone to the tear. Fox et al. [45] reported good results in 90% of cases and Zhang et al. [46,47] showed trephination led to healing of all tears, either partially or fully [47], with an improved healing rate and lower re-tear rate compared with suturing alone [46].
Not all meniscal tears can or should be repaired, particularly if considerable damage has been sustained. Contraindications include: tears located in the inner-third region (zone 3, also known as the white-white zone, where the tissue is entirely devoid of a vascular supply), and tears with major degeneration. Longitudinal tears measuring less than 10 mm in length and incomplete radial tears that do not extend into the outer one-third of the meniscus should also not be repaired. Older patients (above 60 years of age) and those unwilling to follow post-operative rehabilitation programs would also be unsuitable candidates [28].
Degenerative (complex) tears in older patients are among those tears historically treated by unnecessarily invasive means. Sihvonen et al. [48] conducted a randomised sham-controlled trial in patients with a degenerative meniscal tear and no knee OA. Patient outcomes after arthroscopic surgery were no better than those after a sham operation. A subsequent meta-analysis showed a small, clinically insignificant benefit from surgical intervention that is entirely absent within two years [49]. Current evidence does not support a role for arthroscopic debridement, washout, or partial meniscectomy for middle-aged and older patients with knee pain with or without signs of OA [49,50]. First-line treatment comprises non-operative modalities, such as education; self-management; exercise; weight loss, if overweight or obese; walking aids, if indicated, paracetamol; non-steroidal anti-inflammatory drugs; and intra-articular glucocorticoids [50]. Knee pain refractory to conservative therapy may respond to partial meniscectomy in the absence of OA when combined with a physiotherapy program, however, relief does not persist in the long-term [10].
Meniscus replacement
Potential future treatments have expanded their focus beyond the conventional methods. In some cases, there may be an indication to resect and replace the entire meniscus. Meniscal replacement has a greater capacity to protect the joint surfaces and is a suitable option in cases where patients have suffered degenerative changes due to prior meniscectomy or when an irreparable tear is encountered [16]. Meniscal replacement surgery uses natural or synthetic scaffolds to guide tissue repair or regeneration in three dimensions while providing a temporary construct for mechanical function [51]. Clinical application of both allograft transplantation and synthetic replacement scaffolds show promising results [52], however, their superiority to partial meniscectomy still needs to be demonstrated [53].
Conclusion
Meniscal tears are a common orthopaedic pathology that may have an acute traumatic or chronic degenerative cause. Due to the likely complication of OA, alternatives are now preferred to total meniscectomy. There are several surgical approaches suited to treating different patterns of meniscal tear. Where indicated, meniscal repair is the preferred method of treatment, with evidence supporting very good long-term results. When irreparable damage is encountered, removal and replacement of the meniscus with natural or synthetic scaffolds presents a promising option, provided its efficacy can be definitively demonstrated in future trials.
Acknowledgements
The authors wish to acknowledge Hope Orthopaedics for supplying Figure 4 and Figure 5.
Conflicts of interest
None declared.
Correspondence
K Wegrecki: kamil.wegrecki1@my.nd.edu.au
References
[1] Fukubayashi T, Kurosawa H. The contact area and pressure distribution pattern of the knee. A study of normal and osteoarthrotic knee joints. Acta Orthop Scand. 1980;51(6):871-9.
[2] Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14(4):270-5.
[3] Voloshin AS, Wosk J. Shock absorption of meniscectomized and painful knees: a comparative in vivo study. J Biomed Eng. 1983;5(2):157-61.
[4] Mow V, et al. Structure and function relationships of the menisci of the knee, in Knee Meniscus: Basic and clinical foundations, V. Mow, S. Arnoczky, and D. Jackson, Editors. 1992, Raven: New York:p37-57.
[5] Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res, 1975(109):184-92.
[6] Wilson AS, Legg P, McNeur JC. Studies on the innervation of the medial meniscus in the human knee joint. Anat Rec. 1969;165(4):485-91.
[7] Maak TG, Fabricant PD, Wickiewicz TL. Indications for meniscus repair. Clin Sports Med. 2012;31(1):1-14. Epub 2011 Oct 11.
[8] Greis PE, et al. Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg. 2002;10(3):168-76.
[9] Xu C, Zhao J. A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: the more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc. 2015.;23(1):164-70. Epub 2013 May 14.
[10] Howell R, Kumar NS, Patel N, Tom J. Degenerative meniscus: pathogenesis, diagnosis, and treatment options. World J Orthop. 2014;5(5):597-602.
[11] Boyd KT, Myers PT. Meniscus preservation; rationale, repair techniques and results. Knee. 2003;10(1):1-11.
[12] Englund M, Roos EM, Lohmander LS. Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year follow-up of meniscectomy with matched controls. Arthritis Rheum. 2003;48(8):2178-87.
[13] Meredith DS, et al. Factors predicting functional and radiographic outcomes after arthroscopic partial meniscectomy: a review of the literature. Arthroscopy. 2005;21(2):211-23.
[14] Andersson-Molina H, Karlsson H, Rockborn P. Arthroscopic partial and total meniscectomy: A long-term follow-up study with matched controls. Arthroscopy. 2002;18(2):183-9.
[15] Yoon KH, Park KH. Meniscal repair. Knee Surg Relat Res. 2014;26(2):68-76. Epub 2014 May 30.
[16] Hasan J, Fisher J, Ingham E. Current strategies in meniscal regeneration. J Biomed Mater Res B Appl Biomater. 2014;102(3):619-34. Epub 2013 Sep 13.
[17] Shelbourne KD, Dickens JF. Joint space narrowing after partial medial meniscectomy in the anterior cruciate ligament-intact knee. J Am Acad Orthop Surg. 2007;15(9):519-24.
[18] McGinity JB, Geuss LF, Marvin RA. Partial or total meniscectomy: a comparative analysis. J Bone Joint Surg Am. 1977;59(6):763-6.
[19] Jackson JP. Degenerative changes in the knee after meniscectomy. Br Med J. 1968;2(5604):525-7.
[20] Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30B(4):664-70.
[21] Ahmed AM, Burke DL. In-vitro measurement of static pressure distribution in synovial joints–Part I: Tibial surface of the knee. J Biomech Eng. 1983;105(3):216-25.
[22] England M, et al. Meniscal tear in knees without surgery and the development of radiographic osteoarthritis among middle-aged and elderly persons. Arthritis Rheum. 2009;60(3):831-39.
[23] England M, Lohmander LS. Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum. 2004;50(9):2811-19.
[24] Papalia R, et al. Meniscectomy as a risk factor for knee osteoarthritis: a systematic review. Br Med Bull. 2011;99:89-106.
[25] Salata MJ, Gibbs AE, Sekiya JK. A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med. 2010;38(9):1907-16.
[26] Shybut T, Strauss EJ. Surgical management of meniscal tears. Bull NYU Hosp Jt Dis. 2011;69(1):56-62.
[27] Canale S, Beaty J in Campbell’s operative orthopaedics, Campbell’s operative orthopaedics, Mosby, Editor. 2012: St Louis, MO.p.2075-8.
[28] Chatain F, et al. The natural history of the knee following arthroscopic medial meniscectomy. Knee Surg Sports Traumatol Arthrosc. 2001;9(1):15-8.
[29] Noyes FR, Heckmann TP, Barber-Westin SD. Meniscus repair and transplantation: a comprehensive update. J Orthop Sports Phys Ther. 2012;42(3):274-90. Epub 2011 Sep 4.
[30] Heckmann TP, Barber-Westin SD, Noyes FR. Meniscal repair and transplantation: indications, techniques, rehabilitation, and clinical outcome. J Orthop Sports Phys Ther. 2006;36(10):795-814.
[31] Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med. 1982;10(2):90-5.
[32] Cannon Jr WD, Vittori JM. The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med. 1992;20(2):176-81.
[33] Bach Jr. BR, et al. Arthroscopic meniscal repair: analysis of treatment failures. J Knee Surg. 2005;18(4):278-84.
[34] Kimura M, et al. Second look arthroscopy after meniscal repair. Factors affecting the healing rate. Clin Orthop Relat Res. 1995(314):185-91.
[35] Ramappa AJ, et al. A biomechanical evaluation of all-inside 2-stitch meniscal repair devices with matched inside-out suture repair. Am J Sports Med. 2014;42(1):194-9. Epub 2013 Oct 10.
[36] Grant JA, et al. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: a systematic review. Am J Sports Med. 2012;40(2):459-68. Epub 2011 Jul 7.
[37] Boutin RD, Fritz RC, Marder RA. Magnetic resonance imaging of the postoperative meniscus: resection, repair, and replacement. Magn Reson Imaging Clin N Am. 2014;22(4):517-55. Epub 2014 Nov 1.
[38] Mehta V, Terry M. Cyclic testing of 3 all-inside meniscal repair devices: a biomechanical analysis. Am J Sports Med. 2009;37(12):2435-9. Epub 2009 Oct 1.
[39] Starke C, et al. Meniscal repair. Arthroscopy. 2009;25(9):1033-44. Epub 2009 Feb 26.
[40] Rosso C, et al. Comparison of all-inside meniscal repair devices with matched inside-out suture repair. Am J Sports Med. 2011;39(12):2634-9. Epub 2011 Oct 13.
[41] Kurzweil P, Tifford C, Ignacio E. Unsatisfactory clinical results of meniscal repair using the meniscus arrow. Arthroscopy. 2005;21(8):905.
[42] Arnoczky S, Lavagnino M. Tensile fixation strengths of absorbable meniscal repair devices as a function of hydrolysis time. An in vitro experimental study. Am J Sports Med. 2001;29(2):118-23.
[43] Mordecai S, et al. Treatment of meniscal tears: an evidence based approach. World J Orthop. 2014;5(3):233-41. eCollection 2014 Jul 18.
[44] Barber F, et al. FasT-Fix meniscal repair: mid-term results. Arthroscopy. 2008;24(12):1342-8. Epub 2008 Oct 10.
[45] Kotsovolos E, et al. Results of all-inside meniscal repair with the FasT-Fix meniscal repair system. Arthroscopy. 2006;22(1):3-9.
[46] Fox JM, Rintz KG, Ferkel RD. Trephination of incomplete meniscal tears. Arthroscopy. 1993;9(4):451-5.
[47] Zhang Z. Arnold JA. Trephination and suturing of avascular meniscal tears: a clinical study of the trephination procedure. Arthroscopy. 1996;12(6):726-31.
[48] Zhang ZN, et al. Treatment of longitudinal injuries in avascular area of meniscus in dogs by trephination. Arthroscopy. 1988;4(3):151-9.
[49] Sihvonen R, et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369(26):2515-24.
[50] Thorlund JB, Juhl CB, Roos EM, Lohmander LS. Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms. BMJ. 2015. 350:h2747.
[51] Buchbinder R, Harris IA, Sprossen A, Management of degenerative meniscal tears and the role of surgery. BMJ. 2015. 350: h2212.
[52] Moran CJ, et al. Cell distribution and regenerative activity following meniscus replacement. Int Orthop. 2014;38(9):1937-44. Epub 2014 Jul 5.
[53] McCormick F, et al. Survival and reoperation rates after meniscal allograft transplantation: analysis of failures for 172 consecutive transplants at a minimum 2-year follow-up. Am J Sports Med. 2014;42(4):892-7. Epub 2014 Feb 14.
[54] Vrancken AC, Buma P, van Tienen TG. Synthetic meniscus replacement: a review. Int Orthop. 2013;37(2):291-9. Epub 2012 Oct 26.