Child and adolescent psychiatry; an introduction to medical students
Wednesday, April 17th, 2024
Parisa Fani-Molky, Aniqa Hussain, Dr Iain Perkes, Prof. Valsamma Eapen, Prof. Philip Hazell
Available Online: 17/04/2024
Abstract
Introduction: Child and adolescent psychiatry (CAP) is a subspecialty in the field of psychiatry focused on patients aged 0-18 years. CAP is unique, as children rarely seek help on their own, the engagement of parents or carers is always critical for appropriate management, and the relative effectiveness of intervention is unparalleled in clinical medicine.
Summary: Assessment by a child and adolescent psychiatrist is commonly triggered by a request from a general practitioner, paediatrician, school, welfare, or justice service. Management within CAP involves a multidisciplinary approach, including but not limited, to psychological therapy (individual and family), play and art therapy, occupational, speech and other allied health therapy, and pharmacological management. CAP utilises age-defined subspecialties (perinatal and infant, child and adolescent or youth psychiatry) as disorders are expressed differently at varying life stages and require different approaches to management. To attain training within the subspecialty of CAP in Australia and New Zealand, general psychiatry specialty training must first be completed. The outcomes of this CAP training as medical professionals include being able to integrate and apply the medical, developmental, and psychosocial knowledge gained to assist in managing psychopathologies in younger populations.
Key Learning Points:
- Child and adolescent psychiatrists assess patients based on referrals from various sources, examining presenting symptoms, family history, and psychological factors.
- Psychological therapy in CAP is tailored to each age group, and takes into consideration genetic, environmental, and cultural influences.
- Child psychiatrists continue care into young adulthood, emphasizing autonomy and transition to adult services, with a focus on preventing relapse and loss of follow-up.
- Becoming a child and adolescent psychiatrist in Australia involves specialized training, including completing an advanced certificate through RANZCP, with prerequisites and experiences in general psychiatry and CAP settings.
Introduction
There has been a cultural shift towards holistic care in modern medicine due to recent understandings regarding the various interconnections between physical and psychological health. However, the field of psychiatry has always understood the importance of holistically treating patients and basing treatment on a comprehensive assessment considering a patient’s biological, psychological (cognitive), family, financial, and cultural factors. This is particularly important in the subspecialty of child and adolescent psychiatry (CAP). Not only must we consider a child’s family, but also the developmental life stages and environments in which children interact. CAP focuses on a comprehensive bio-psychosocial assessment, justifying treatment plans which apply different modes of therapy to promote optimal mental health and quality of life.
It is estimated that one in seven Australian children aged between four and 17 experienced mental illness within the previous year [1]. However, as children may not be able to seek help by themselves, it is incumbent upon carers, school staff or agencies to recognise mental health issues in children and seek treatment on their behalf. Unfortunately, there has been a steady increase in the mental health needs of children and adolescents in Australia and New Zealand [2]. For example, the demand for hospital mental health admissions were 25-55% higher than predicted from July to November 2020 [2]. However, with the substantial increase in demand, their needs are not being adequately met due to a shortage of child and adolescent psychiatrists [3]. One factor influencing this shortage is a lack of awareness regarding CAP. Thus, we aim to summarise one common and one less common psychopathology seen and the unique clinical challenges faced across different age groups (early childhood, middle childhood, adolescence and transitioning to adult care). This is to highlight the importance of flexibility and adjusting clinical practise to best suit each patient to optimise overall outcomes. Additionally, we outline the basics of the CAP training pathway, with the aim to increase medical students’ understanding and appreciation of CAP.
Background
Assessments by child and adolescent psychiatrists are commonly triggered by a request from a general practitioner, paediatrician, school, welfare, or justice service [4,5]. The assessment of the child involves the clinician ascertaining the presenting symptoms and interacting with the child and relevant carers to obtain a developmental and family history and assess the mental, cognitive and behavioural state of the child [4-6]. A cognitive assessment by a psychologist and an assessment of speech and language, motor, sensory and daily living skills by allied health members and reports from the school form part of the bio-psychosocial assessment. A 2018 study conducted by Segal et al. examined the prevalence of CAP service usage in South Australia. It was found that from infancy to age 15, prevalence ranged from 5.3-7.6%, whereas in adolescence it increased to 16.3% [7]. Thus, it is essential to tailor therapeutic approaches for each age group as the prevalence of psychopathologies increases with adolescence [7].
Psychological therapy within CAP involves individual, family and group therapies, as well as psychotropic medication; the treatment mode recommended is dependent on service availability, patient preferences and clinical assessment and findings [8]. The main objective of the assessment is to ascertain the nature of the presenting complaint, precipitants, and its impact on the child’s life [4,5]. To establish a formulation regarding the current predicament, the clinician will consider both the child’s genetic predispositions, physical health, exposures from in utero through adolescence, and temperamental and cognitive traits and their wider environmental context, including parental mental health and the home and cultural factors like migration or indigenous heritage [4-6]. This approach aims to address any intergenerational trauma that may exist and other maladaptive behaviours that may have stemmed from their environments.
Overview of psychiatry in infancy and early childhood (0–5 years)
Social functioning evolves rapidly during the first three years of life, and infants vary considerably in their temperament [4,9]. Disorders with an onset in the first years of life usually reflect a disturbed infant-care relationship, in the context of parental mental illness, neurodevelopmental problems or other underlying medical conditions [4,6]. Infants with higher demands may place increased stress on carers, potentially compounding distress in both the infant and carer [4]. Hence, we have discussed both attachment disorders and autism spectrum disorders (ASD) within the context of early childhood psychiatry and appropriate clinical approaches.
Attachment disorders are thought to stem from an impairment between the infant and the parent to form healthy attachments [4,6,10,11]. Risk factors include parental mental illness such as maternal post-natal depression, neglect, abuse, abrupt separation from carers or frequent changes in care [11]. Assessment is age-specific and carried out by applying the ‘Strange Situation’ scenario where the child is separated from their carer, introduced to a stranger and then reunited with the carer with careful observation of behaviour [4]. Management of attachment problems includes therapies that focus on strengthening the relationship between primary caregivers and the infant to improve understanding of each other’s emotions in addition to programs focused on parenting skills with parent child psychotherapy and attention to feeding, sleeping and health difficulties of both caregiver and child [4].
Autism spectrum disorder (ASD) is one of a group of neurodevelopmental disorders that is characterised by social communication and interaction abnormalities together with restricted and repetitive patterns of behaviour [4,10,12]. Longitudinal cranial imaging studies have found excessive cortical thickening in early development, followed by cortical thinning during adolescence [4]. Those with ASD may present with stereotypic and repetitive behaviours, difficulty adapting to new situations, cognitive, social and communicative delays and differences [4,10,12]. Management consists of a multidisciplinary approach, including behavioural management, social skills training and carer support [4,12]. Individuals with ASD frequently experience other neurodevelopmental disorders such as attention deficit hyperactivity disorder (ADHD) as well as comorbid mood disorders such as anxiety and depression [10]. Second-generation antipsychotics have a role in reducing disruptive behaviours and dysregulation in extreme cases but must be used cautiously due to adverse cognitive and metabolic side-effects [4,12].
Overview of psychiatry in middle childhood (6–12 years)
The primary school years see children moving their focus away from ties with their carers, beginning to explore complex relationships with others and acquiring social skills which will equip them to meet the social and learning demands of their school and peers [4]. They start developing ‘prosocial’ behaviour and empathy, including sharing and helping peers in distress [4]. Learning difficulties in these prosocial behaviours can disrupt the achievement of age-specific goals and may cause long-term implications, such as a mismatch between abilities and scholastic demands [4,9]. Two examples of psychopathologies that may appear within this age group are ADHD and conduct disorders and the differing clinical approaches required is generally discussed below.
ADHD is a neurodevelopmental disorder that manifests with developmentally excessive hyperactivity, distractibility, impulsivity and inattentiveness in multiple settings [4,10,13]. Children may have predominantly poor concentration (inattentive subtype), or overactivity and impulsivity (hyperactive-impulsive subtype) or a combined-type ADHD [4,10,13]. Functional neuroimaging shows underactivity in the frontal lobes, the caudate nucleus and overactivity in the amygdala [4]. Serial MRI studies show widespread, delayed thickening in cortical structures compared with controls [4]. Management is multimodal, with behavioural counselling, classroom strategies, parent education and central nervous system stimulants such as methylphenidate and amphetamine [4, 13]. The use of medication must be regularly reviewed for therapeutic response and side-effects.
Conduct disorder (CD) is described by repeated bullying, deception, thieving, cruelty and violence to people or animals, not better explained by another condition [4,10,14]. Early signs of aggression and defiance can be seen in children as young as two years old; however, an isolated antisocial act does not warrant the diagnosis [4,14]. There is reduced amygdala activity in response to frightening faces in those with callous-unemotional traits compared with those without; this hypoactivity is contrasted with amygdala hyperactivity (compared with healthy controls) in cases of CD without callous-unemotional attributes [4]. Established CD resists change, so early intervention is crucial [4]. Multisystemic therapy that utilises social and emotional learning and cognitive behavioural therapy (CBT) helps to reduce behavioural symptoms while selective use of antipsychotics and mood stabilisers can also be helpful [4, 14]. About half the children with CD will manifest an antisocial personality pattern or related psychopathology in adulthood [4, 14].
Overview of psychiatry in adolescence (13–18 years)
Adolescence is a phase of profound changes in social relationships, body morphology,
responsibilities, and personality traits [4,9]. These changes reflect a shift to a more autonomous role and greater internal control, the hallmarks of adult functioning [4]. Many serious psychiatric disorders—schizophrenia spectrum disorder, substance abuse, mood disorders, borderline personality disorder, anorexia and bulimia nervosa—can have their onset during this period, although there is often a developmental history of emotional and behavioural problems during childhood [4,9].
Although depression can occur in young children, its incidence increases in adolescence [4,15]. Depression is gradual in onset and may present atypically, with irritability, hypersomnia or binge eating [4,10,15]. Comorbidity is common, particularly with behaviour problems, substance abuse and anxiety. One in 10 adolescents suffers a major depressive episode that meets diagnostic criteria and leads to functional impairment [4,15]. Still, only a small proportion are accurately diagnosed and treated [4]. While mild symptoms may remit spontaneously, persistent mild to moderate symptoms require and are usually responsive to psychological treatment. Antidepressant medications are less effective than in adults but are prescribed in more severe cases with active monitoring of response and side-effects [4,15].
Schizophrenia, presenting with psychotic symptoms such as delusions and hallucinations, usually has its onset in late adolescence to mid-twenties and is exceptionally in those younger [4,10,16]. Prodromal symptoms include mood and behavioural changes, with obsessional thinking and odd beliefs [4,10,16]. When psychotic symptoms first manifest, organic aetiologies of psychosis such as central nervous system abnormalities, intoxication, metabolic derangements, and immune-mediated conditions need to be ruled out [4,16]. Treatment is multidisciplinary, including second-generation antipsychotics, psychological therapy and social support as well as psychoeducation for carers [4,16].
There is a clear evidence base for individual psychotherapy in children and adolescents including CBT, interpersonal psychotherapy, dialectical behavioural therapy, and mindfulness-based therapy depending on the psychopathology and cognitive ability [4]. Family therapy is utilised when structural or communication difficulties manifest within the family [4]. When assessing adolescents, the clinician may offer to see the patient on their own and then involve the parents [4,5]. Prior to this, confidentiality, and its limits—if there is risk of harm to the patient or third party—should be discussed with the adolescent [4]. Informed consent is required from parents and adolescents over 15 years of age, however children under 15 years of age can ‘assent’ to treatment but is not necessary when there is parental consent [4]. Regardless, a graded approach is used, and explanations are tailored to the patient’s intellectual and emotional capacity. Parents and children are provided psychoeducation regarding the nature of the condition and its recommended treatments [4,8]. Goals are formed in a collaborative manner by identifying specific behaviours or problems in both the home and outside environments [4].
Overview of psychiatry in young adulthood (18-25 years)
Although this demographic does not fit into childhood, child and adolescent psychiatrists may continue care of these patients due to factors such as a lack of resources and urgency of care. Clinical trial data specific to this age group is difficult to ascertain as it is usually captured in the age range of 18 to 65 years. However, a large focus in this age group is on transition of care to adult services [4]. The young person is now expected to act autonomously and manage themselves which may prove to be difficult [4]. Transition to adult care is more likely to succeed if they are jointly supported by both CAP and adult facilities during this period to prevent relapse, recurrence, or loss to follow up [4].
Pathway to a career in CAP
Child and adolescent psychiatrists need to complete a Certificate of Advanced Training of the Royal Australian and New Zealand College of Psychiatrists (RANZCP). Entry to CAP in Australia and New Zealand is via a RANZCP accredited general psychiatry training program and hospital/mental health service registrar employment (minimum five years) (Figure 1) [3,17]. All general psychiatry trainees undertake a six-month term in CAP, usually in the second or third year of training [3,16]. To specialise in CAP and complete the Certificate of Advanced Training, senior psychiatry trainees then spend their final 24 months of training in accredited CAP training posts, where they will be exposed to a full range of child and adolescent mental health conditions [3,17]. However, they can also complete the full five years of general psychiatry and graduate as a Fellow of the RANZCP and then subsequently decide to do CAP training [3,17]. The Advanced Certificate of CAP training involves placement in a community and inpatient setting (at least 6 months each), together with the accredited program of specialist education and the option to complete a research project [3,17]. There is no exit examination for CAP, but trainees are required to satisfactorily complete several work-based assessments during the two years of subspecialty training [3,17]. Figure 2 outlines a resource list for those interested in learning more about CAP in Australia and New Zealand.
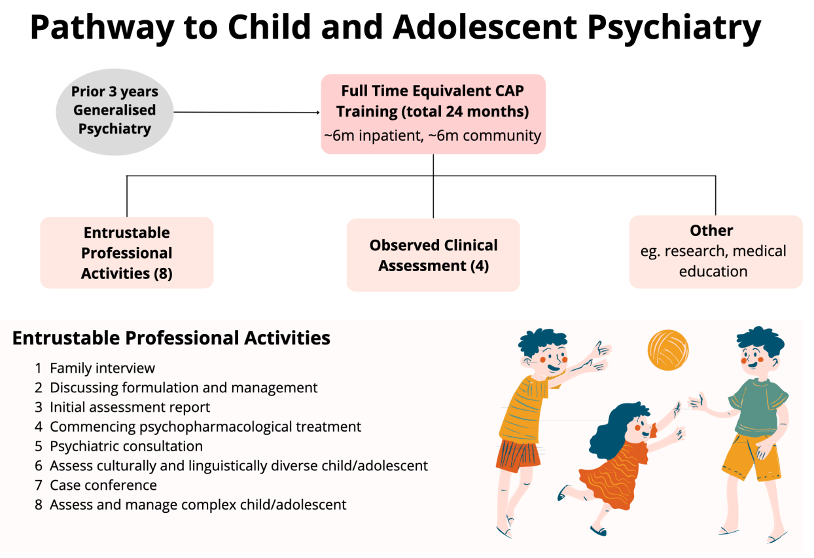
Figure 1. The pathway to child and adolescent psychiatry. After three years of training in general psychiatry, trainees complete two years of subspecialist training, including of both inpatient and community settings. Four observed clinical assessments and eight entrustable professional activities are completed to demonstrate clinical competency.

Figure 2. Resources for emerging child and adolescent psychiatrists in Australia and New Zealand. The International Association for Child and Adolescent Psychiatry and Allied Professions (IACAPAP) is a free e-textbook of Child and Adolescent Mental Health, written by an international group of child and adolescent psychiatrists and allied professionals. The Psychiatry Interest Forum (PIF) provides information and opportunities for medical students and junior doctors interested in psychiatry. The Faculty of Child and Adolescent Psychiatry (FCAP) of the Royal Australian and New Zealand College of Psychiatrists (RANZCP) advises on training, clinical practice, and research. The Foundations of Clinical Psychiatry (4th Edition) is an introductory textbook for medical students and covers all fields of psychiatry from a biological, psychological, and social lens.
Conclusion
CAP is a dynamic subspecialty focused on early intervention with the aim of providing better long-term mental health outcomes for children and their families. A key benefit of intervening early through CAP is the impact medical practitioners can have in improving the trajectory of a child and their family’s lives. The outcomes of CAP training for medical professionals include being able to integrate and apply the knowledge gained within their training to the comprehensive assessment of childhood psychopathology and deliver targeted treatments and management plans. Through this, they will be able to facilitate effective service delivery for children, adolescents and their families and help them navigate the various multifaceted and complex dilemmas faced by children requiring psychiatric care.
References
- Mental health services in Australia Australian Institute of Health and Welfare. 2022. Available from: https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia/report-content/prevalence-impact-and-burden-of-mental-health?fbclid=IwAR0fvPYWrkdCAWKlC0POYvaZCVj-Rdgn5sgK6UfCVDIDFP0bEP6DWMJdfH0
- Hu N, Nassar N, Shrapnel J, Perkes I, Hodgins M, O’Leary F, et al. The impact of the COVID-19 pandemic on paediatric health service use within one year after the first pandemic outbreak in New South Wales Australia – a time series analysis. Lancet Reg Health West Pac. 2022;19:100311. doi: 10.1016/j.lanwpc.2021.100311
- Perkes IE, Eggleston M, Jacobs B, McEvoy P, Fung D, Robertson PG. The making of child and adolescent psychiatrists in Australia and New Zealand. Australian and New Zealand journal of psychiatry. 2021:486742110556-48674211055654. doi: 10.1177/00048674211055654
- Hazell P, Perkes IE. Child and Adolescent Psychiatry. In: Bloch S, et al., editor. Foundations of Clinical Psychiatry Fourth Edition. Melbourne, Australia: Melbourne University Publishing; 2017. p. 366-92.
- Lempp T, Lange Dd, Radeloff D, Bachmann C. The clinical examination of children, adolescents and their families. In: Rey JM, editor. IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions; 2012.
- Mares S, Woodgate S. The clinical assessment of infants, preschoolers and their families. In: Rey JM, editor. IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions; 2017.
- Segal, L., Guy, S., Leach, M., Groves, A., Turnbull, C., Furber, G., 2018. A needs-based workforce model to deliver tertiary-level community mental health care for distressed infants, children, and adolescents in South Australia: a mixed-methods study. The Lancet Public Health 3, e296–e303. doi:10.1016/s2468-2667(18)30075-6
- Lorberg B, Davico C, Martsenkovskyi D, Vitiello B. Principles in using psychotropic medication in children and adolescents. In: Rey JM, editor. IACAPAP Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions; 2019.
- IACAPAP Textbook of Child and Adolescent Mental Health. Rey JM, editor. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions; 2012.
- Diagnostic and statistical manual of mental disorders : DSM-5-TR. 5th edition, text revision. ed. Washington, DC: American Psychiatric Association Publishing; 2022.
- Erikson, Erik H. Childhood and Society. 2nd ed. London, England: Triad, 1977.
- Fuentes J, Bakare M, Munir K, Aguayo P, Gaddour N, Öner Ö. Autism spectrum disorder. In: Rey JM, editor. IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions; 2014.
- Sousa AdFd, Coimbra IM, Castanho JM, Polanczyk GV, Rohde LA. Attention deficit hyperactivity disorder. In: Rey JM, Martin A, editors. JM Rey’s IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions; 2020.
- Scott S. Conduct disorders. In: Rey JM, editor. IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions; 2012.
- Rey JM, Bella-Awusah TT, Liu J. Depression in children and adolescents. In: Rey JM, editor. IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions; 2015.
- Starling J, Feijo I. Schizophrenia and other psychotic disorders of early onset. In: Rey JM, editor. IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions; 2012
- Certificate of Advanced Training in Child and Adolescent Psychiatry: The Royal Australian and New Zealand College of Psychiatrists. 2015. Available from: https://www.ranzcp.org/pre-fellowship/about-the-training-program/certificates-of-advanced-training/child-and-adolescent-psychiatry
