4th Year MBBS, Griffith University
School refusal: identification and management of a paediatric challenge
Sarah Nguyen
Thursday, August 31st, 2017
4th Year MBBS, Griffith University
School refusal is not truancy, but both are serious behavioural problems that can have detrimental consequences. Management of school refusal involves ruling out organic causes and assessing contributing factors, such as anxiety and depression. Empirical treatment involves a collaborative approach of cognitive and behavioural therapies involving the child, parents, and school. This article highlights the heterogeneous nature of school refusal, its identification, assessment and management, and the implications for future research.
Introduction
At first glance, school refusal appears to be a relatively straightforward phenomenon that all youth may experience at some point during their school years. However, youth-motivated school absence is a significant public health problem affecting schools and households around Australia. Nationally, the average attendance rate of state secondary school students is approximately 85%, with the Northern Territory experiencing the lowest rate of attendance at 75% [1]. In Queensland, an estimated 30% of state secondary school students had an attendance rate below 90%, or had missed more than 20 days of school over one school-year [2]. Of the reasons given, ‘unexplained’ absences accounted for more than 25% of the total absences [3]. Due to financial and legal issues associated with chronic absenteeism, health professionals are put under increasing pressure by parents and schools to find a solution to the child’s ‘problem.’ This strain may lead doctors to write generic medical certificates or practice ‘defensive medicine’ in order to avoid professional and legal risks.
Definition
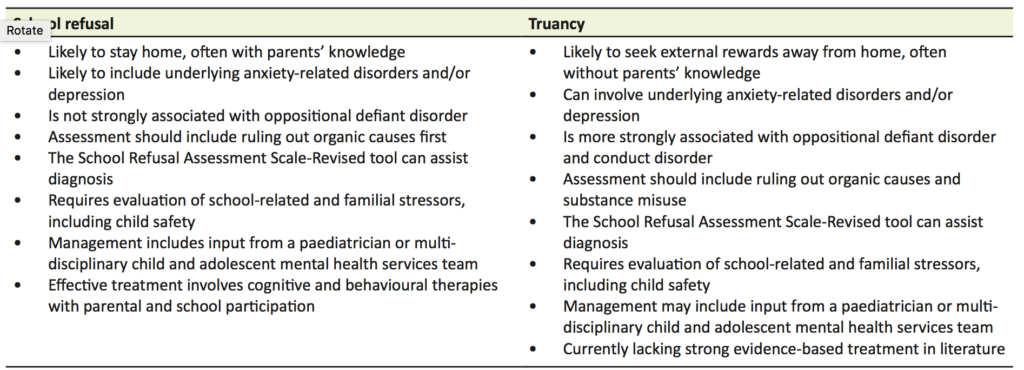
School refusal is not a psychiatric diagnosis, but rather a symptom that encompasses a range of possible diagnoses or social problems. There are many terms in the literature that are used to describe the different types of absenteeism. Firstly, child-motivated absenteeism differs from ‘school withdrawal’ in that the latter refers to situations where a family deliberately keeps their child at home for various reasons, such as due to financial reasons or to care for an ill family member [4]. Child-motivated absenteeism is typically categorised into those with school refusal and those displaying truancy (Table 1). ‘School refusal’ is generally thought to encompass difficulties attending or staying in school, and is associated with extreme emotional distress [4–7]. The child stays home with their parents’ knowledge, despite the parents having made a reasonable attempt to encourage the child to attend school. Children exhibiting truancy, in contrast, are more likely to display antisocial tendencies, such as vandalism and theft, rather than emotional distress [4–7]. Truants’ motives for absenteeism include a lack of interest in school-work, unwillingness to conform to the school’s code of behaviour, and an over-riding desire to engage in externalising behaviour, such as disruptive acts or alternative tangible reinforcers on a school day [4–7]. In addition, parents are often unaware of or disinterested in their child’s school absence. The separation of absenteeism into school refusal and truancy has been criticised for the bias shown to children with school refusal who are often perceived sympathetically and judged to be worthy of treatment, while the term ‘truant’ raises punitive connotations and the need for discipline [8,9]. Due to this bias, children labelled truants are under-represented in current literature and it is unclear whether interventions differ between this group and children with school refusal, particularly due to a lack of strong supporting evidence with regards to the effectiveness of common psychological treatments in groups with externalising behaviour, such as truancy [10,11]. Groups inclusive of differing causes of absenteeism should be a future research objective. Until then, since management of school absenteeism is critical for all youth, it is therefore important to be aware of this bias and assess each child individually and thoroughly.
Epidemiology
Approximately 1–5% of all school-aged children will demonstrate school refusal behaviour at some point [6,7]. Although it can occur at any age, school refusal is more common between 5–7 years and 12–14 years of age. These age groups correspond to periods of transition to primary and secondary school, respectively [7]. The prevalence of school refusal seems to be unaffected by gender, socio-economics or intelligence [7,12]. One study showed that a high prevalence of adolescents with school refusal and co-morbid depression also experienced learning difficulties, which may have been a causal factor in their school refusal [13]. In a study assessing parental and familial risk factors for school refusal in children, physical punishment by parents, history of organic disease in parents or the child, and positive psychiatric history in a parent or relative were found to be significant [14]. There have been conflicting arguments in the literature regarding the role of family dysfunctions such as conflict, strict parenting or isolation, and school refusal [15,16]. These various aetiological factors emphasise the heterogeneous nature underlying school refusal and the necessity for future studies with larger sample sizes to assist in delineating predisposing risk factors.
Clinical features
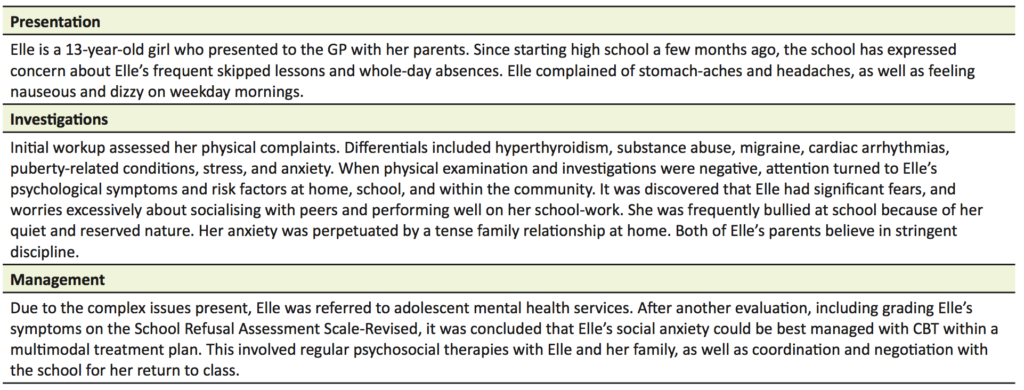
The onset of school refusal can occur acutely, such as on the first day of a new school term, or gradually, such as increasing reluctance to attend school until outright school refusal. Non-attendance can occur sporadically, or continually for weeks or months [6]. The emotional distress that often accompanies school refusal can manifest behaviourally, physiologically, and cognitively [6,7]. Behaviours include remaining in bed, refusing to leave the car, crying, or having temper tantrums. Physiological symptoms include abdominal pain, nausea, vomiting, headaches, diarrhoea, sore throat, sweating, and frequent urination. On a cognitive level, children often have irrational fears about school attendance [7]. A case example of school refusal outlining the presentation, investigations, and management is included (Table 2).
Chronic school refusal has a strong association with anxiety-related disorders [17,18]. Common diagnoses include separation anxiety disorder, generalised anxiety disorder, social phobia, specific phobia, and adjustment disorder with anxiety [7,18]. There appears to also be age-related trends in regards to the diagnoses, for example younger children are often assessed to have separation anxiety whereas adolescents tend to be diagnosed with phobias [7]. These phobias are often in relation to social situations where there is an irrational fear of being criticised. People with an anxiety-related disorder often have co-morbid depression; and certainly, there is a high prevalence of school refusal in children with diagnosed or sub-clinical depression [18].
Children with school refusal can also display argumentative and aggressive behaviour when pressure is exerted upon them to attend school. This type of externalising behaviour leads to many of these children being diagnosed with oppositional defiant disorder [7]. It is important to note that in school refusal, this externalising behaviour is not displayed in multiple settings, but primarily contained to the home environment. By definition, conduct disorder-type behaviours, such as social disregard and violence, are not characteristic of school refusal, but more often associated with truancy.
Assessment
As with any clinical presentation, a thorough history and medical examination must be taken to rule out organic causes. Only reasonable investigations relevant to the presenting physical symptoms should be conducted [19]. Obviously, if a chronic medical condition were to be uncovered, the primary focus of management would be appropriate referral and education [20].
In addition to a detailed history of the presenting physical symptoms, a health practitioner should consider the predisposing, precipitating, and perpetuating issues of the child’s school refusal in terms of individual, family, school, and community factors. Attention should be given to the family function, the reactions and responses of those surrounding the child to their school refusal, and peer relationships in school [19]. Liaising with the school for information about the child’s attendance records and academic progress would be useful to look for trends in absenteeism and potentially undiagnosed learning difficulties. In addition to days missed, it is also important to enquire about tardiness, early departures from school, missed lessons, and time spent out of class. Discussion about the child’s behaviour and social interactions are vital to exclude victimisation from bullying [21].
Formal assessment
Standardised behavioural checklists and mental health scales can be given to the child, their parents, and the school teachers to assist in delineating problems and comparing the severity of behaviours at school and home [19]. The School Refusal Assessment Scale-Revised (SRAS-R) is one of the widely accepted checklists used internationally to assess the functional model of school refusal behaviour, such as positive and negative reinforcements [22]. Determining the functional profile of school-refusing behaviour can also assist in identifying underlying psychiatric diagnoses [23]. The SRAS-R has been verified as having good validity, reliability, and utility [5,24]. However, a recent study has highlighted the ambiguity of certain items on the SRAS-R and suggests that some questions should be removed for improved validity and reliability [25]. The use of the scale can be extended across more generalised populations of school absenteeism, including truancy [26].
Child safety
Finally, health practitioners should be wary of the possibility of an unsafe home situation that the child may be exposed to, as this can contribute to school refusal. For example, a child may feel anxious and hesitant about leaving home if they feel the need to portray a protective role for a parent under domestic violence [20]. Mandatory reporting laws exist in all Australian states and territories for suspected cases of child abuse and neglect. Given the slight differences amongst states regarding child abuse legislation and protocol, it is advisable to check the details applicable to your jurisdiction [27]. Provisions within legislation protect practitioners from liability for reporting confidential information if the report was made in good faith. If a practitioner is uncertain about reporting, they can contact the local child protection unit or a paediatrician for discussion and advice [28].
Prognosis
A quarter of refusals are estimated to remit spontaneously or are dealt with successfully by the family and school without practitioner intervention [5]. However, school refusal has detrimental consequences for the majority of the remaining cases that go undetected and unmanaged. Short-term consequences include poor academic performance, family conflict, and damaged peer relationships. Long-term outcomes include social isolation, employment issues, and increased risk of ongoing internalising mental health problems and developing a psychiatric illness in adulthood, such as panic disorder and agoraphobia [19,29]. On first presentation, risk factors that indicate a poorer prognosis of returning to school consist of severe or long-standing school refusal, being adolescent or of older age, and having a co-morbid psychiatric illness, particularly depression [7,19].
Although there is a strong emphasis on a timely return to school for refusers, few published studies are available that report the long-term implications of return to school. One study concluded that there was enduring improvement in family relationships after the resolution of the child’s school refusal, however, there appeared to be no difference in the long-term social or emotional adjustment [30]. Another retrospective study found long-term improvement in educational and employment outcomes after school refusal treatment, except for those diagnosed with social phobia and learning difficulties; however, the study was limited by small sample size [31]. Further controlled studies investigating the long-term functional impact of managing school refusal need to be conducted.
Treatment
The primary objective of treatment for youth displaying school refusal is timely return to school. Behavioural therapies and cognitive behaviour therapy (CBT) have been widely studied and accepted as first line treatment where school refusal is associated with the primary diagnosis of an anxiety disorder [32–37]. Unfortunately, studies are limited by high treatment drop-out rates and inconsistent results on follow-up [33,37]. There is also a lack of randomised controlled trials investigating interventions other than CBT variants, such as group therapy or hypnotherapy [32,38,39]. These limitations indicate the need for future research with better-controlled studies and reproducible results, as well as considering other intervention types. More recent studies have found that CBT is most likely to be successful when it is incorporated into a multimodal treatment method involving the child, parents, and school [40,41]. Due to its heterogeneous nature, some cases of school refusal can be complex and persistent, therefore it is recommended that the child be referred to a paediatrician or to child and adolescent mental health services, which include inter-disciplinary teams, for holistic long-term management, which might include medication.
The child
Child treatment plans should be individually tailored, depending on the psychological basis of their school refusal as well as their developmental level [42]. This may initially include relaxation training for those with substantial physiological manifestations of anxiety. By reducing feelings of anxiety, children are better engaged to utilise various CBT strategies. Cognitive therapy can be used to scope the relationship between a child’s emotions and their behaviour, and ultimately facilitate school attendance by problem-solving and modifying maladaptive cognitions [7,43]. Social skills training is beneficial in addressing any deficits in social skills, which may be contributing to the school refusal, as well as managing the social anxiety associated with talking about their absence to peers or teachers [43]. Improving communication between parent and child is also an important component of CBT. Ultimately, graded exposure and planned return to school should be encouraged, involving the child and their teacher with modification of schoolwork and improved in-class support. Regular positive reinforcement should be used to assist progression, and monitoring for relapse is essential.
The parents
Parental and family support is crucial for successful return to school. It has been observed that improvement can be made only through positive influence and when the child is convinced that their parents are determined to achieve regular school attendance [44]. Parents should be taught to employ contingency plans and behaviour management strategies, such as ignoring inappropriate behaviour and positively reinforcing appropriate behaviours. Heeding signs of parental psychopathology and initiating anxiety management education may also help parents maintain their composure and focus when facilitating their child’s school attendance [7,43]. This may include arranging for parents to receive mental health services or marital therapy.
The school
The practitioner and parents should also closely liaise with the child’s school in order to enable a smooth return to school. It is important to educate school staff about school refusal behaviour and associated psychological issues, to dispel potential misconceptions about students with school attendance difficulties. School staff are encouraged to accommodate special arrangements, including modifying schoolwork and assessment, and allowing graduated attendance, such as only coming in for favourite lessons or for the first part of the day. Supportive teachers and ‘peer buddies’ are recommended to ensure the child’s experience of school is positive [43]. Complaints of somatic symptoms should be treated tentatively, and unless the child is clearly unwell, they should remain at school.
Pharmacotherapy
Pharmacological treatment may be considered adjunct to the cognitive and behavioural therapies, especially when the child has severe underlying anxiety or depressive symptoms, or when they have not responded to the comprehensive psychosocial treatments offered [45]. Based on existing clinical trial studies, there is little satisfactory evidence that supports the effectiveness of commonly prescribed medications. There appears to be some evidence favouring the tricyclic anti-depressant (TCA), imipramine, with concomitant psychosocial therapy as a superior therapy to placebo combined with psychosocial therapy [46–48]. Short-term outcomes consisted of improved school attendance and reduction in anxiety and depressive symptoms [47]. These positive findings were not maintained in a naturalistic one-year follow up study [48]. TCAs can be problematic due to their unpleasant side-effects and toxicity, including cardiovascular complications [49]. Selective serotonin reuptake inhibitors (SSRI), such as fluoxetine, have weaker evidence of efficacy for school-refusing children, showing no significant difference in therapeutic efficacy between combined CBT-and-fluoxetine therapy and CBT alone [50–52]. Despite this, SSRIs tend to be favourable in practice as they are shown to be effective in reducing depressive symptoms in children and adolescents, and are less likely to cause serious adverse effects [52–54]. Children on medication require regular review for response and side-effects.
Conclusions
School refusal is a challenging problem for health practitioners, families, and schools. Early identification and management reduces the risk of detrimental short- and long-term consequences. Management of school refusal can be complicated and arduous, and needs active participation from the child’s parents and school, as well as possibly paediatricians and mental health services. The preferred management of school refusal involves a multimodal treatment approach and CBT. There should be more awareness and understanding about this mental health risk and the potential for early intervention to promote the health and wellbeing of the future generations.
School refusal is a growing topic of interest in the literature. However, the current literature is largely limited by selection of the absentee population, lack of intervention types, poor sample sizes and follow-up, conflicting outcomes, and lack of long-term sequelae after return to school. In order to establish the efficacy of school refusal interventions, future research could benefit from further adequately powered randomised controlled studies with independent reproducible results. There should also be a focus on investigating groups with different causes of absenteeism, such as truancy, as well as management modalities other than CBT and their long-term effects.
Acknowledgements
My thanks to the Mt Gravatt Child and Youth Mental Health Service for their mentoring and inspiration for this review. Thanks to Dr Randal Moldrich (University of Queensland) for a critical review of the manuscript.
Conflicts of interest
None declared.
References
[1] Australian Curriculum, Assessment and Reporting Authority. National report on schooling in Australia 2012. Table 17, Student attendance rates, government schools, by year level, sex and state and territory, 2012 (per cent); student attendance rates, government schools, by year level and state and territory, 2008–11 (per cent); [cited 2016 March 26]. Available from: http://www.acara.edu.au/verve/_resources/20151210_ANR_2012_Additional_Statistics_w_Part_9.pdf
[2] Department of Education, Training and Employment. Performance insights: school attendance. Queensland: Queensland Government; 2013 [cited 2016 March 8]. Available from: http://education.qld.gov.au/everydaycounts/docs/performance-insights-report.pdf
[3] Department of Education and Training. School attendance: Absences by reason and school [spreadsheet on the internet]. 2015 [cited 2016 March 8]. Available from: http://education.qld.gov.au/schools/statistics/student-attendance.html
[4] Kearney C. School absenteeism and school refusal behavior in youth: a contemporary review. Clin Psychol Rev 2008;28(3):451-71.
[5] Elliott J. Practitioner review: School refusal: issues of conceptualisation, assessment, and treatment. J Child Psychol Psychiatry 1999;40(7):1001-12.
[6] Tonge B, Cooper H, King N, Heyne D. School refusal: description and management. Current Therapeutics 2002;43(3):55-61.
[7] Heyne D, King NJ, Tonge BJ, Cooper H. School refusal: epidemiology and management. Paediatr Drugs 2001;3(10):719-32.
[8] Lyon A, Cotler S. Towards reduced bias and increased utility in the assessment of school refusal behaviour: The case for diverse samples and evaluations of context. Psychol Sch 2007;44(6):551-65.
[9] Brandibas G, Jeunier B, Clanet C, Fouraste R. Truancy, school refusal and anxiety. Sch Psychol Int 2004;25(1):117-26.
[10] Southam-Gerow M, Kendall P. Cognitive-behaviour therapy with youth: advances, challenges and future directions. Clin Psychol Psychother 2000;7(5):343-366.
[11] Maynard B, McCrea K, Pigott T, Kelly M. Indicated truancy interventions for chronic truant students: a Campbell systematic review. Res Soc Work Pract 2013;23(1):5-21.
[12] Hampe E. Miller L, Barrett C, Noble H. Intelligence and school phobia. Y Sch Psychol 1973;11(1):66-70.
[13] Naylor M, Staskowski M, Kenney M, King C. Language disorders and learning disabilities in school-refusing adolescents. J Am Acad Child Adolesc Psychiatry 1994;33(9):1331-7.
[14] Bahali K, Tahiroglu AY, Seydaoglu. Parental psychological symptoms and familial risk factors of children and adolescents who exhibit school refusal. East Asian Arch Psychiatry 2011;21(4):164-9.
[15] Bernstein G, Borchardt C. School refusal: Family constellation and family functioning. J Anxiety Disord 1996;10(1):1-19.
[16] Bernstein G, Garfinkel B. Pedigrees, functioning, and psychopathology in families of school phobic children. Am J Psychiatry 1988;145(1):70-4.
[17] Jones A, Suveg C. Flying under the radar: School reluctance in anxious youth. School Ment Health 2015;7(3):212-23.
[18] Egger H, Costello J, Angold A. School refusal and psychiatric disorders: a community study. J Am Acad Child Adolesc Psychiatry 2003;42(7):797-807.
[19] Sewell J. School refusal. Aust Fam Physician 2008;37(6):406-8.
[20] Katz F, Leith E, Paliokosta E. Fifteen-minute consultation for a child not attending school: a structured approach to school refusal. Arch Dis Child Educ Pract Ed 2016;101(1):21-5.
[21] Havik T, Bru E, Ertesvag S. School factors associated with school refusal- and truancy-related reasons for school non-attendance. Soc Psychol Educ 2015;18(2):221-40.
[22] Kearney C. Identifying the function of school refusal behavior: A revision of the school refusal assessment scale. J Psychopathol Behav Assess 2002;24(4):235-45.
[23] Kearney C, Albano A. The functional profiles of school refusal behaviour: Diagnostic aspects. Behav Modif 2004;28(1):147-61.
[24] Ingles CJ, Gonzalvez-Macia C, Garcia-Fernandez JM, Vicent M, Martinez-Monteagudo MC. Current status of research on school refusal. European Journal of Education and Psychology 2015;8(1):37-52.
[25] Heyne D, Vreeke L, Maric M, Boelens H, Van Widenfelt. Functional assessment of school attendance problems: an adapted version of the school refusal assessment scale-revised. J Emot Behav Disord [Internet]. 2016 [cited 2016 Oct 26]; Available from: http://ebx.sagepub.com/content/early/2016/07/26/1063426616661701.full.pdf+html DOI: 10.1177/1063426616661701
[26] Haight C, Kearney C, Hendron M. Confirmatory analyses of the school refusal assessment scale-revised: replication and extension to a truancy sample. J Psychopathol Behav Assess 2011;33(2):196-204.
[27] Mathews B, Scott D. Mandatory reporting of child abuse and neglect [Internet]. Australia: Australian Institute of Family Studies; 2014 [cited 2016 March 26]. Available from: https://aifs.gov.au/cfca/publications/mandatory-reporting-child-abuse-and-neglect
[28] Bird S. Child abuse: Mandatory reporting requirements. Aust Fam Physician. 2011;40(11):921-6.
[29] Flakierska-Praquin N, Lindstrom M, Gillberg C. School phobia with separation anxiety disorder: a comparative 20- to 29-year follow-up study of 35 school refusers. Compr Psychiatry 1997;38(1):17-22.
[30] Valles E, Oddy M. The influence of a return to school on the long-term adjustment of school refusers. J Adolesc 1984;7(1):35-44.
[31] McShane G, Walter G, Rey J. Functional outcome of adolescents with ‘school refusal.’ Clin Child Psychol Psychiatry 2004;9(1):53-60.
[32] Maynard B, Brendel K, Bulanda J, Heyne D, Thompson A, Pigott T. Psychosocial interventions for school refusal with primary and secondary school students: a systematic review. Syst Rev 2015;11(12).
[33] Beidas R, Crawley S, Mychailyszyn M, Comer J, Kendall P. Cognitive-behavioral treatment of anxious youth with comorbid school refusal: clinical presentation and treatment response. Psychological Topics 2010;19(2):255-71.
[34] King N, Tonge B, Heyne D, Ollendick T. Research on the cognitive-behavioral treatment of school refusal: a review and recommendations. Clin Psychol Rev 2000;20(4):495-507.
[35] Blagg N, Yule W. The behavioural treatment of school refusal: a comparative study. Behav Res Ther 1984;22(2):119-27.
[36] Heyne D, Sauter F, Van Widenfelt B, Vermeiren R, Westenberg P. School refusal and anxiety in adolescence: non-randomised trial of a developmentally sensitive cognitive behavioral therapy. J Anxiety Disord 2011;25(7):870-8.
[37] Maric M, Heyne D, MacKinnon D, Van Widenfelt B, Westernberg P. Cognitive mediation of cognitive-behavioural therapy outcomes for anxiety-based school refusal. Behav Cogn Psychother 2013;41(4):549-64.
[38] Aviv A. Tele-hypnosis in the treatment of adolescent school refusal. Am J Clin Hypn 2006;49(1):31-40.
[39] Sahel R. Group counselling/therapy as a technique to modify the undesirable school behaviour (school phobia) of children at elementary school level in the state of Kuwait [dissertation on the internet]. Bangor, UK: Prifysgol Bangor University; 1989. [cited 2016 Oct 26]. Available from: http://e.bangor.ac.uk/4189/
[40] Reissner V, Jost D, Krahn U, Knollmann M, Weschenfelder A, Neumann A, et al. The treatment of school avoidance in children and adolescents with psychiatric illness. Dtsch Arztebl Int 2015;112(39):655-62.
[41] Oner O, Yurtbasi P, Er A, Basoglu N. The inpatient treatment process for severe school refusal. Klinik Psikofarmakol Bülteni 2014;24(2):176-9.
[42] Bares C. Emerging metacognitive processes during childhood: implications for intervention development with children. Child Adolesc Social Work J 2013;28(4):291-9.
[43] Heyne D, Rollings S. School refusal. Cornwall: Blackwell Publishers Ltd; 2002.
[44] Berg I. Absence from school and mental health. Br J Psychiatry 1992;161(2):154-66.
[45] Tonge B. Pharmacotherapy of school refusal. Behav Change 1998;15(2):98-106.
[46] Layne A, Bernstein G, Egan E, Kushner M. Predictors of treatment response in anxious-depressed adolescents with school refusal. J Am Acad Child Adolesc Psychiatry 2003;42(3):319-26.
[47] Bernstein G, Borchardt C, Perwien A, Crosby P, Kushner M, Thuras P, et al. Imipramine plus cognitive-behavioural therapy in the treatment of school refusal. J Am Acad Child Adolesc Psychiatry 2000;39(3):276-83.
[48] Bernstein G, Hektner J, Borchardt C, McMillan M. Treatment of school refusal: one-year follow-up. J Am Acad Child Adolesc Psychiatry 2001;40(2):206-13.
[49] Geller B, Reising D, Leonard H, Riddle M, Walsh T. Critical review of tricyclic antidepressant use in children and adolescents. J Am Acad Child Adolesc Psychiatry 1999;38(5):513-6.
[50] Tonge T, Melvin G, Dudley A, Clarke K, Gordon M. The augmentation of cognitive behavioural therapy with fluoxetine for the treatment of adolescent school refusal: a randomised controlled trial. Neuropsychiatr Enfance Adolesc 2012;60(5):S297.
[51] Wu X, Liu F, Cai H, Huang L, Li Y, Mo Z, et al. Cognitive behaviour therapy combined fluoxetine treatment superior to cognitive behaviour therapy alone for school refusal. Int J Pharm 2013;9(3):197-203.
[52] Melvin G, Dudley A, Gordon M, Klimkeit, Gullone E, Taffe J, et al. Augmenting cognitive behavior therapy for school refusal with fluoxetine: a randomised controlled trial. Child Psychiatry Hum Dev [Internet]. 2016 [cited 2016 Oct 26]; Available from: https://www.ncbi.nlm.nih.gov/pubmed/27485100 DOI: 10.1007/s10578-016-0675-y
[53] Qin B, Zhang Y, Zhou X, Cheng P, Liu Y, Chen J, et al. Selective serotonin reuptake inhibitors versus tricyclic antidepressants in young patients: a meta-analysis of efficacy and acceptability. Clin Ther 2014;36(7):1087-95.
[54] Korczak D. Use of selective serotonin reuptake inhibitor medications for the treatment of child and adolescent mental illness. Paediatr Child Health (Oxford) 2013;18(9):487-91.

