Saving behaviour cleans hands: A reflection on the behavioural psychology of hand hygiene
Raelene Aw-Yong
Wednesday, December 2nd, 2015
Since the time of Semmelweis, it has long been realised that hands are the commonest vehicles for the spread of hospital-acquired infections (HAI). If all transmission opportunities, as defined by the World Health Organisation (WHO), were met with proper hand hygiene, the current incidence of HAIs could reduce by more than half. [1-3] Unfortunately, almost every hospital fails at this. Globally, the diverse roots of noncompliance in healthcare workers (HCWs) need to be tackled in a multifactorial way. Lack of resources, high-intensity workloads and ignorance about hand hygiene necessity or technique are often first to be blamed and rightly so, according to large studies in multiple countries. [4-6] However, in most Australian hospitals where regularly-replenished hand hygiene products sit at every bedside and informative posters are abound on corridor walls, compliance still remains at 82.2&. [7] Ajzen’s Theory of Planned Behaviour (TPB) proposes that it is not only the factors external to the individual, such as those aforementioned, but also internal behavioural factors that shape an individual’s hand hygiene practices. [8] These internal factors, often less explored than external factors, will be the topic of discussion.
Centrality of Intention
The central thesis of TPB is this: the likelihood of performing a voluntary behaviour is best predicted by the intention to do it. [8] According to Ajzen, intention is the extent of effort one is willing to go to in order to achieve that action. [8] A 2012 Cochrane review and a landmark hand hygiene behavioural study by O’Boyle et al. demonstrates this positive association between intention and behavioural achievement. [15,16] Even so, it is imperative early in this discussion that we not assume that self-reported scores are good measures of actual compliance; in reality, the association is demonstrably poor because external factors do commonly prevent intention from actualising as behaviour. [15,17] However, external factors are not the focus here.
Intention is determined by three secondary internal factors – attitude, social norm and perceived behavioural control – that are, in turn, a function of beliefs based on one’s information about a behaviour. [14] We will now explore these factors in detail.
Attitude
Attitudes derive from an individual’s cognitive and emotional evaluation of behaviour. This evaluation, in turn, depends on the various positive or negative attributes and consequences the individual has associated with the behaviour. If HCWs perceive positive attributes about hand hygiene, the desirable attitudes this yields increases their levels of intention and correlate well with compliance. [6,14,15] One’s perceptions hinge on one’s beliefs about a behaviour. [14,15] Based on a focus group study of 754 nurses and a 2006 review, beliefs about hand hygiene can originate inherently or electively and account for 64% and 76%, respectively, of variation in intention. [18]
Inherent beliefs
During most individuals’ childhoods, exposure of hands to ‘dirtiness’ becomes ritualised as a trigger for disgust and the subsequent urge to cleanse one’s hands. Consequently, inherent patterns develop. [18-20] The toilet-training years may see a solidification of positive attitudes towards hand hygiene behaviours specifically in situations where individuals feel the instinctual need to ‘emotionally cleanse’ themselves. [18] This positive association appears consistent across diverse demographic groups. [21] However, what varies is each individual’s tolerance threshold of contamination before they feel the urge to cleanse, in accordance with culture, exposure to education and environment. [1] The 500 Australian respondents to a 2008 international hygiene beliefs survey on average scored one of the lowest levels of concern about “getting sick because of poor hygiene” and “being infected in contact with other people”. [22] Yet, a similar survey found that Australians do still place a strong emphasis on handwashing. [23] In reality, the hand hygiene standards promoted by Australian culture in general may be suboptimal to what is actually required for microbiological protection. It is common for nurses to only feel compelled to wash their hands after becoming ‘emotionally soiled’ from touching patients’ axillae, groins, genitals or excretions, if visibly contaminated, or from feeling moist or gritty, but not in other situations. [18] Although long-standing, developmentally-based inherent beliefs about dirtiness are possibly the most challenging of the psychological factors to address, one intervention could be the incorporation of emotionally evocative themes and slogans in infection control campaigns.
Compliance figures also suffer when the inherent belief associating hand hygiene with self-protection is undermined by products that have caused users pain, discomfort and/or the occasional hypersensitivity reaction. With the transition to the standardised use of emollient-containing alcohol-based handrubs (ABHR) across Australian healthcare facilities since 2008, the skin damage, irritation and dryness associated with handwashing with soap have dramatically reduced. [24-26] Although the addition of emollients to the ABHR solutions has greatly reduced associated stinging sensations and contact dermatitis, ABHRs remain painful to use for some, most likely due to improper use, having split or cracked skin, or allergic dermatitis. [26] Whatever the reason, the formation of new inherent beliefs that emotionally link pain and discomfort with correct hand hygiene behaviour continually works to worsen behavioural compliance. [1,27] It seems the only way to address this problem is to await advances in dermatological products in order to further enhance the dermal tolerance of ABHRs.
Elective beliefs
On the other hand, elective attitudes originate from beliefs that deliver the schema of hand hygiene over to choice. Elective beliefs measure various hand hygiene behaviours according to a less intuitive outcome of a higher order – microbiological self-protection proved by objective laboratory evidence. The opportunities for hand hygiene just after HCWs touch ‘emotionally clean’ parts of patients or inanimate surroundings, autoclaved equipment, hospital telephones or computers are the key targets of these elective beliefs. [18] Inherent disgust alone cannot be relied upon to stimulate enough intention in HCWs to engage in appropriate disinfection during these situations. Indeed, it is no surprise that hand hygiene opportunities that specifically relate to elective beliefs are the ones most frequently neglected by nurses, especially during peaks in workload. [18]
It seems the solution is not as simple as correcting inaccurate elective beliefs. In contrast with the way inherent beliefs naturally permeate one’s attitudes, translating elective beliefs into attitudes is often met with resistance. [18] Although the best targets for change would be unique for every HCW, some common determinants affecting elective belief-to-attitude translation have been identified. Firstly, elective beliefs regarding hand hygiene opportunities at work also tend to mirror hygiene beliefs about corresponding out-of-hospital situations. The more concerned a HCW is about handwashing before preparing a meal or after stroking pets or using a computer, the more likely they are to have positive attitudes about using the proper hand hygiene after ‘emotionally clean’ events at work. [18] Notably, the previously mentioned 2008 hygiene beliefs survey demonstrated Australians were amongst those who expressed the lowest concern for “hand hygiene while cooking and eating”. [22] Perhaps, infection control campaigns could be made more effective by challenging the household habits and beliefs of HCWs in addition to their usual chastisements targeting scenarios within the work context.
Secondly, although this subject requires further research, religious attitudes concerning hand cleansing rituals could also influence the elective beliefs of Buddhist, Hindu, Muslim and Orthodox Jewish HCWs. They are encouraged, if not commanded, to clean their hands for hygiene, usually following ‘unclean’ acts and meals. [1] Additionally, having a community-oriented mindset in favour of protecting others would also strengthen positive attitudes towards hand hygiene. [1] Although less than 7.3% of the Australian population affiliate with these religions and much of Western society tends towards individualistic ideals, [28] these findings could assist local campaigns in areas where there are more individuals within these target groups, for example, at hospitals located in culturally and linguistically diverse suburbs.
Lastly, a more modifiable aspect of elective beliefs that could strengthen good attitudes is having a solid understanding of the scientific evidence proving the microbiological protectiveness of hand hygiene. [20] Most awareness campaigns rely heavily on the positive association between good knowledge, belief in the strong efficacy of hand hygiene practices, and compliance. [1] The Australian National Hand Hygiene Initiative recommends “evidence-based education on all aspects of hand hygiene in healthcare” for student HCWs, and for local initiatives to help HCWs “understand the evidence underlying the recommendation” to use ABHRs. [29]
The evidence is up-to-date and irrefutable, the studies too countless to ignore. Proper hand hygiene curtails HAI rates dramatically. [3,30-38] Yet, despite awareness campaigns and convenient online access to the major literature, HCWs (mostly in developed nations) still cite the lack of convincing evidence as their reason for non-compliance. [18,20] There are several common reasons for this. The evidence base does lack randomised controlled trials (RCTs) that are hospital-based and double-blinded. However, such studies are unfeasible; it is impossible to blind subjects from their own hand hygiene practices, implementing a control group would clearly be unethical to patients, and it is extremely difficult to simulate a realistic hospital working environment (the lack of which may confound results). [39] Nevertheless, ample community-based open RCTs and cluster trials have produced sufficiently convincing, high-quality results. [40-44] Another common objection blames ABHRs for increasing the incidence of Clostridium difficile-associated diseases. However, this has long been epidemiologically refuted. [1,32,45-49] Perhaps the deepest reason why it is not sufficient to simply educate HCWs about the evidence of the benefits to patients is this – being convinced about the self-protective efficacy of elective hand hygiene motivates many HCWs much more than knowing its patient-protective efficacy does. This attitude has been a recurrent finding across the various age groups, levels of employment experience and backgrounds of scientific training. [18,20] It may do well for awareness campaigns to place even greater emphasis on evidence demonstrating the self-protective nature of hand hygiene.
Subjective Norm
The second determinant of intention is subjective norm – the perception of how positively hand hygiene is endorsed by the people one respects within the workplace. [15,50] Staff members viewed as role models have the greatest impact on a HCW’s subjective norm. In 2009, Erasmus et al. conducted focus group studies on 65 nurses, consultants, junior house officers and medical students across five hospitals. Although their study was Netherlands-based, Erasmus et al.’s analysis of the social norm dynamics occurring within a hospital environment still offers key insights into the interplay between subjective norms and compliance for Australian HCWs. The study subjects most commonly identified doctors and experienced nurses, such as nurse managers, as their role models for clinical practice. [20] Another study also identified hospital administrators as role models. [18] At a busy neonatal intensive care unit, staff intention to practise good hand hygiene significantly increased when senior staff members’ opinions on the practice were perceived to be more favourable. [51] Thus, mass improvement could be found in encouraging the role models of each workplace to be thoughtful in their speech, ideas and habits, especially when around their colleagues.
Conversely, Erasmus et al. also highlighted how negative role models have the greatest power over medical students and junior nurses. [20] Perhaps this is because junior members of the healthcare team are frequently the most sensitive and feel that their behavioural control (explored in the next section) is being limited whenever subjective norms are defined by negative role models. [52] For example, in the study, many medical students believed they were unable to satisfactorily disinfect their hands between seeing patients on ward rounds because they would otherwise fall behind the rest of the team. Furthermore, in attempts to assimilate into their working environments, students admitted to imitating hospital staff, particularly doctors, without questioning their actions first. These findings demonstrate how the cycle of noncompliance could persist from one generation of role models to the next. [20] It is possible that the pressure on students to imitate senior HCWs could arise from the heuristic method of teaching common in medical schools, as well as the professional expectation that senior doctors mentor junior doctors. Being encouraged to learn from supervisors opportunistically, students often slip into the habit of accepting all advice unfiltered. Students may benefit from being regularly reminded of this pitfall by their clinical preceptors.
Peer HCWs, although not role models, may also degrade subjective norms in a hospital by contributing to its ‘culture’ of noncompliance. A negative subjective norm rooted in so widespread an acceptance of noncompliance can inform the elective beliefs and attitudes of less-experienced HCWs who may be more vulnerable to believing whatever they observe to be correct. [20] A cross-sectional survey of 2961 staff revealed that doctors and nurses experienced a strong direct association between intention and peer pressure from within their own respective professions. [53]
There have been many interventional attempts to nurture a culture of compliance. Many Australian hospitals have designated ‘hand hygiene champions’ as culture-enforcers and role models. Infection control teams design encouraging posters and use frequent audits with feedback to staff in attempts to stimulate inter-ward competitiveness and a sense of shared responsibility about compliance. However, a subculture of resistance to these strategies has emerged. [54] It is not uncommon to hear staff comment with an undertone of rebellion, “I wash my hands for extra long when the infection control police are around.”
Perceived Behavioural Control
The third independent determinant of intention, perceived behavioural control, describes one’s self-perceived likelihood of performing an action. [15,51] As part of a focus group study, Australian nurses identified the most common external influences on their control over hand hygiene performance. Many felt they lacked the relevant training in infection control. They reported that regular education programs and simple “Five Moments” charts placed around wards would avert any growing misconceptions about the need for disinfection after touching patient surroundings and remind them when they forget or get distracted. [55] During peaks in busyness or emergencies, HCWs have also indicated having no time to adhere to every moment of hand hygiene. Other times, when in the middle of performing certain tasks, they may feel unable to interrupt the activity to go clean their hands midway. Lastly, disapproval of hand hygiene by senior staff, mostly doctors, was discussed as a salient issue in focus group studies. All these factors were negatively associated with intention, measured by self-reported compliance. [6,20,53,55,56]
There is an important distinction between one’s perceived control, dependent on internal cognisance of how external factors affect one’s behaviour, and the actual ability of control they have been afforded by these external factors; the two commonly differ. [57] The link between actual ability and internal cognisance is self-efficacy. For an individual already familiar with infection control theory and technique, self-efficacy manifests as the confidence to actually practise what they have learnt when it is required. Alternatively, interventions seeking to increase self-efficacy of HCWs who find themselves constrained by time restrictions or the overbearing opinions of senior staff may involve improving HCW assertiveness, knowledge about hospital policy regarding patient safety, and practise in escalating concerns with other staff. [57] Training could involve testing a student’s capacity to remind a HCW to decontaminate their hands after observing them failing to do so while on the wards. [57]
Summary
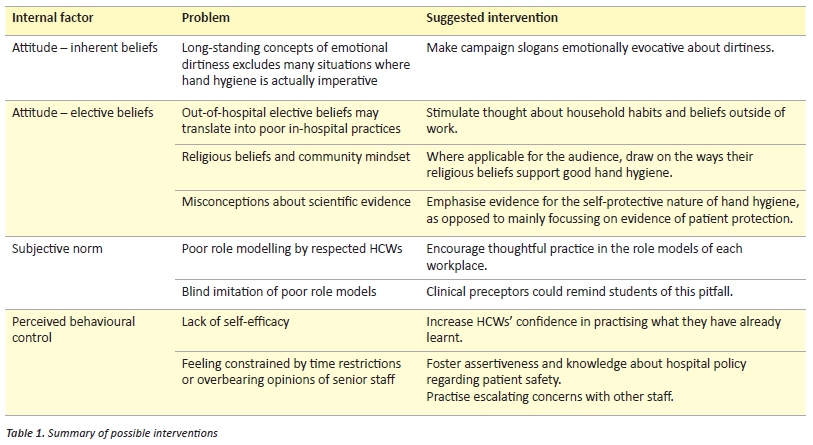
Why is it that HCWs fail to clean their hands? Using the TPB framework, we explored the internal behavioural factors underlying noncompliance. HCWs’ beliefs about hand hygiene are informed by elements both at work and in the community. These perceptions define attitude, subjective norms and perceived behavioural control, which predict intention to clean one’s hands. With this understanding, it is imperative that interventions addressing compliance do not ignore these modifiable influences on HCWs. Table 1 is a summary of interventions suggested in this article. Addressing the behavioural psychology of hand hygiene might just be the final nail in the coffin for hand-transmitted HAIs.
Acknowledgements
None.
Conflict of interest
None declared.
Correspondence
R Aw-Yong: raelene.awyong@my.jcu.edu.au
References
[1] World Health Organisation. WHO Guidelines on Hand Hygiene in Health Care. Geneva: World Health Organisation; 2009.
[2] Martin-Madrazo C, Cañada-Dorado A, Salinero-Fort MA, Abanades-Herranz JC, Arnal-Selfa R, Garcia-Ferradal I et al. Effectiveness of a training programme to improve hand hygiene compliance in primary healthcare. BMC Pub Health. 2009;9:469.
[3] Grayson ML, Jarvie LJ, Martin RL, Johnson PD, Jodoin ME, McMullan C et al. Significant reductions in methicillin-resistant Staphylococcus aureus bacteraemia and clinical isolates associated with a multisite, hand hygiene culture-change program and subsequent successful statewide roll-out. Med J Aust. 2008;188(11):633-40.
[4] Wisniewski MF, Kim S, Trick WE, Welbel SF, Weinstein RA, Chicago Antimicrobial Resistance Project. Effect of education on hand hygiene beliefs and practices: a 5-year program. Infect Control Hosp Epidemiol. 2007;28(1):88-91.
[5] Widmer AF, Conzelmann M, Tomic M, Frei R, Stranden AM. Introducing alcohol-based hand rub for hand hygiene: the critical need for training. Infect Control Hosp Epidemiol. 2007;28(1):50-4.
[6] Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV. Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med. 2004;141(1):1-8.
[7] Hand Hygiene Australia. National Data Period 1, 2015. Canberra: Hand Hygiene Australia; 2015. http://www.hha.org.au/LatestNationalData/national-data-2015.aspx.
[8] Ajzen I. From Intentions to Actions: A Theory of Planned Behaviour. In: Kuhl J, Beckmann J, eds. Action Control: From Cognition to Behaviour. Germany: Springer; 1985:11-39.
[9] Clayton DA, Griffith CJ. Efficacy of an extended theory of planned behaviour model for predicting caterers’ hand hygiene practices. Int J Environ Health Res. 2008;18(2):83-98.
[10] Gronhoj A, Bech-Larsen T, Chan K, Tsang L. Using Theory of Planned Behaviour to predict healthy eating among Danish adolescents. Health Educ. 2012;112(1):4-17.
[11] Rhodes RE, Blanchard CM, Matheson DH. A multicomponent model of the theory of planned behaviour. Br J Health Psychol. 2006;11(Pt1):119-37.
[12] Swanson V, Power KG. Initiation and continuation of breastfeeding: theory of planned behaviour. J Adv Nurs. 2005;50(3):272-82.
[13] Carmack C, Lewis-Moss R. Examining the Theory of Planned Behaviour Applied to Condom Use: The Effect-Indicator vs. Causal-Indicator Models. J Prim Prev. 2009;30(6):659-76.
[14] Ajzen I. The Theory of Planned Behaviour. Organ Behav Hum Decis Process. 1991;50:179-211.
[15] O’Boyle CA, Henly SJ, Larson E. Understanding adherence to hand hygiene recommendations: the theory of planned behaviour. Am J Infect Control. 2001;29(6):352-60.
[16] Huis A, van Achterberg T, de Bruin M, Grol R, Schoonhoven L, Hulscher M. A systematic review of hand hygiene improvement strategies: a behavioural approach. Implement Sci. 2012;7:92.
[17] Jenner EA, Fletcher BC, Watson P, Jones FA, Miller L, Scott GM. Discrepancy between self-reported and observed hand hygiene behaviour in healthcare professionals. J Hosp Infect. 2006;63(4):418-22.
[18] Whitby M, McLaws ML, Ross MW. Why healthcare workers don’t wash their hands: a behavioural explanation. Infect Control Hosp Epidemiol. 2006;27(5):484-92.
[19] Curtis V, Biran A, Deverell K, Hughes C, Bellamy K, Drasar B. Hygiene in the home: relating bugs and behaviour. Soc Sci Med. 2003;57(4):657-72.
[20] Erasmus V, Brouwer W, van Beeck EF, Oenema A, Daha T, Richardus JH. A qualitative exploration of reasons for poor hand hygiene among hospital workers: lack of positive role models and of convincing evidence that hand hygiene prevents cross-infection. Infect Control Hosp Epidemiol. 2009;30(5):415-9.
[21] Curtis V, Cairncross S. Effect of washing hands with soap on diarrhoea risk in the community: a systematic review. Lancet Infect Dis. 2003;3(5):275-81.
[22] Hygiene Matters: The SCA Hygiene Report 2008. Stockholm: Svenska Cellulosa Aktiebolaget; 2008. http://www.sca.com/Documents/en/Publications/SCA%20Hygiene%20matters_ENG.pdf?epslanguage=en.
[23] Women and Hygiene: The SCA hygiene matters report 2011. Stockholm: Svenska Cellulosa Aktiebolaget; 2010. http://www.sca.com/Documents/en/Publications/SCA-Hygiene-Matters-2011.pdf.
[24] Picheansathian W. A systematic review on the effectiveness of alcohol-based solutions for hand hygiene. Int J Nurs Pract. 2004;10(1):3-9.
[25] Kampf G, Wigger-Alberti W, Schoder V, Wilhelm KP. Emollients in a propanol-based hand rub can significantly decrease irritant contact dermatitis. Contact Derm. 2005;53(6):344-934.
[26] Graham M, Nixon R, Burrell LJ, Bolger C, Johnson PD, Grayson ML. Low rates of cutaneous adverse reactions to alcohol-based hand hygiene solution during prolonged use in a large teaching hospital. Antimicrob Agents Chemother. 2005;49(10):4404-5.
[27] Boyce JM, Pittet D. Guideline for Hand Hygiene in Health-Care Settings: Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Soc Healthcare Epidemiol Am/Assoc Prof Infect Control/Infect Dis Soc Am. MMWR Recomm Rep. 2002;51(RR-16):1-45, quiz CE1-4.
[28] Australian Bureau of Statistics. 2071.0 – Reflecting a Nation: Stories from the 2011 Census, 2012-2013. Canberra: Australian Bureau of Statistics; 2013. http://www.abs.gov.au/ausstats/abs@.nsf/mf/2071.0.
[29] Grayson ML, Russo P, Ryan K, Havers S, Heard K. Hand Hygiene Australia Manual 2013: 5 Moments for Hand Hygiene. Canberra: Hand Hygiene Australia; 2013.
[30] World Health Organisation. Evidence of hand hygiene to reduce transmission and infections by multi-drug resistant organisms in health-care settings. Geneva: World Health Organisation; 2014. http://www.who.int/gpsc/5may/MDRO_literature-review.pdf.
[31] Grayson ML, Russo PL, Cruickshank M, Bear JL, Gee CA, Hughes CF et al. Outcomes from the first 2 years of the Australian National Hand Hygiene Initiative. Med J Aust. 2011;195(10):615-9.
[32] McLaws ML, Pantle AC, Fitzpatrick KR, Hughes CF. Improvements in hand hygiene across New South Wales public hospitals: clean hands save lives, part III. Med J Aust. 2009;191(8 Suppl):S18-24.
[33] Allegranzi B, Pittet D. Role of hand hygiene in healthcare-associated infection prevention. J Hosp Infect. 2009;73(4):305-15.
[34] Roberts SA, Sieczkowski C, Campbell T, Balla G, Keenan A, Auckland District Health Board Hand Hygiene Steering and Working Groups. Implementing and sustaining a hand hygiene culture change programme at Auckland District Health Board. N Z Med J. 2012;125(1354):75-85.
[35] Jarlier V, Trystram D, Brun-Buisson C, Fournier S, Carbonne A, Marty L et al. Curbing methicillin-resistant Staphylococcus aureus in 38 French hospitals through a 15-year institutional control program. Arch Intern Med. 2010;170(6):552-9.
[36] Stone SP, Fuller C, Savage J, Cookson B, Hayward A, Cooper B et al. Evaluation of the national Cleanyourhands campaign to reduce Staphylococcus aureus bacteraemia and Clostridium difficile infection in hospitals in England and Wales by improved hand hygiene: four year, prospective, ecological, interrupted time series study. BMJ. 2012;344:e3005.
[37] Pittet D, Hugonnet S, Harbarth S, Mourouga P, Sauvan V, Touveneau S. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet. 2000;356(9238):1307-12.
[38] Huang GK, Stewardson AJ, Grayson ML. Back to basics: hand hygiene and isolation. Curr Opin Infect Dis. 2014;27(4):379-89.
[39] Jumaa PA. Hand hygiene: simple and complex. Int J Infect Dis. 2005;9(1):3-14.
[40] Nicholson JA, Naeeni M, Hoptroff M, Matheson JR, Roberts AJ, Taylor D et al. An investigation of the effects of a hand washing intervention on health outcomes and school absence using a randomised trial in Indian urban communities. Trop Med Int Health. 2014;19(3):284-92.
[41] Suess T, Remschmidt C, Schink SB, Schweiger B, Nitsche A, Schroeder K et al. The role of facemasks and hand hygiene in the prevention of influenza transmission in households: results from a cluster randomised trial; Berlin, Germany, 2009-2011. BMC Infect Dis. 2012;12:26.
[42] Savolainen-Kopra C, Haapakoski J, Peltola PA, Ziegler T, Korpela T, Anttila P et al. Hand washing with soap and water together with behavioural recommendations prevents infections in common work environment: an open cluster-randomized trial. Trials. 2012;13:10.
[43] Hübner NO, Hübner C, Wodny M, Kampf G, Kramer A. Effectiveness of alcohol-based hand disinfectants in a public administration: impact on health and work performance related to acute respiratory symptoms and diarrhoea. BMC Infect Dis. 2010;10:250.
[44] Sandora TJ, Taveras EM, Shih MC Resnick EA, Lee GM, Ross-Degnan D et al. A randomized, controlled trial of a multifaceted intervention including alcohol-based hand sanitizer and hand-hygiene education to reduce illness transmission in the home. Pediatrics. 2005;116(3):587-94.
[45] Boyce JM, Ligi C, Kohan C, Dumigan D, Havill NL. Lack of association between the increased incidence of Clostridium difficile-associated disease and the increasing use of alcohol-based hand rubs. Infect Control Hosp Epidemiol. 2006;27(5):479-83.
[46] Vernaz N, Sax H, Pittet D, Bonnabry P, Schrenzel J, Harbarth S. Temporal effects of antibiotic use and hand rub consumption on the incidence of MRSA and Clostridium difficile. J Antimicrob Chemother. 2008;62(3):601-7.
[47] Kaier K, Hagist C, Frank U, Conrad A, Meyer E. Two time-series analyses of the impact of antibiotic consumption and alcohol-based hand disinfection on the incidences of nosocomial methicillin-resistant Staphylococcus aureus infection and Clostridium difficile infection. Infect Control Hosp Epidemiol. 2009;30(4):346-53.
[48] McDonald LC, Owings M, Jernigan DB. Clostridium difficile Infection in Patients Discharged from US Short-stay Hospitals, 1996–2003. Emerg Infect Dis. 2006;12(3):409-15.
[49] Archibald LK, Banerjee SN, Jarvis WR. Secular trends in hospital-acquired Clostridium difficile disease in the United States, 1987-2001. J Infect Dis. 2004;189(9):1585-9.
[50] Tai JW, Mok ES, Ching PT, Seto WH, Pittet D. Nurses and physicians’ perceptions of the importance and impact of healthcare-associated infections and hand hygiene: a multi-center exploratory study in Hong Kong. Infection. 2009;37(4):320-33.
[51] Pessoa-Silva CL, Posfay-Barbe K, Pfister R, Touveneau S, Perneger TV, Pittet D. Attitudes and perceptions toward hand hygiene among healthcare workers caring for critically ill neonates. Infect Control Hosp Epidemiol. 2005;26(3):305-11.
[52] Grube JW, Morgan M, McGree ST. Attitudes and normative beliefs as predictors of smoking intentions and behaviours: a test of three models. Br J Soc Psychol. 1986;25(Pt 2):81-93.
[53] Sax H, Uçkay I, Richet H, Allegranzi B, Pittet D. Determinants of good adherence to hand hygiene among healthcare workers who have extensive exposure to hand hygiene campaigns. Infect Control Hosp Epidemiol. 2007;28(11):1267-74.
[54] Tropea J, Clinical Epidemiology & Health Service Evaluation Unit Royal Melbourne Hospital. A national stakeholder review of Australian infection control programs: the scope of practice of the infection control professional (Final draft report). Sydney: Australian Commission on Safety and Quality in Healthcare; 2008.
[55] White KM, Jimmieson NL, Obst PL, Graves N, Barnett A, Cockshaw et al. Using a theory of planned behaviour framework to explore hand hygiene beliefs at the ‘5 critical moments’ among Australian hospital-based nurses. BMC Health Serv Res. 2015;15(59); doi: 10.1186/s12913-015-0718-2.
[56] Ajzen I. Attitudes, Personality, and Behaviour: Mapping social psychology. Berkshire, England: McGraw-Hill International; 2005.
[57] Van de Mortel T. Development of a questionnaire to assess healthcare students’ hand hygiene knowledge, beliefs and practices. Aust J Adv Nurs. 2009;26(3):9-16.