Adequacy of anticoagulation according to CHADS2 criteria in patients with atrial fibrillation in general practice – a retrospective cohort study
Dr. Skye Macleod
Tuesday, September 1st, 2015
Background: Atrial fibrillation (AF) is a common arrhythmia associated with an increased risk of stroke. Strategies to reduce stroke incidence involve identification of at-risk patients using scoring systems such as the CHADS2 score (Congestive Heart Failure, Hypertension, Age ≥75 years, Diabetes or Stroke) to guide pharmacological prophylaxis. Aim: The aim of this research project was to determine the prevalence and management of AF patients within the general practice (GP) setting and to assess the adequacy of anticoagulation or antiplatelet prophylaxis according to the CHADS2 score. Methods: This study was a retrospective cohort study of 100 AF patients ≥50 years conducted at a South Coast NSW Medical Centre over a 3-year period. Data was obtained from existing medical records. CHADS2 scores were determined at baseline, 12 months and 3 years and were compared with medications to assess whether patients were undertreated, adequately treated or over-treated according to their CHADS2 score. Results: Prevalence of AF in patients >50 years was 5.8%. At baseline, 65% of patients (n=100) were at high risk of stroke (CHADS2 score ≥2). This increased to 75.3% of patients at 12 months (n=89) and 78.4% of patients at 3 years (n=60). Adequate treatment occurred in 79.0% of patients at baseline and 83.1% and 76.7% at 12 months and 3-years, respectively. There were three instances of stroke or trans-ischemic attack during the study period. Conclusion: GPs play a critical role in prevention of stroke in patients with AF. Adequate pharmacological interventions occurred in the majority of cases, however, identification and treatment of at-risk patients could be further improved.
Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmia in Australia, affecting 8% of the population over the age of 80 years. [1,2] The morbidity and mortality associated with AF is primarily due to an increased risk of thromboembolic events such as stroke, with studies reporting up to a five-fold increase in the annual risk of stroke among patients with AF who have not received prophylaxis with either anticoagulant or antiplatelet therapies. [3,4]
It has been demonstrated that the incidence of stroke in patients with AF can be significantly reduced with the use of pharmacological agents, such as anticoagulant and antiplatelet medications including warfarin and aspirin, respectively. [5] More recently, the development of new oral anticoagulant (NOAC) medications such as dabigatran and rivaroxaban have also been approved for use in patients with AF. [6] However, several studies indicate that the use of anticoagulants and antiplatelets for the prevention of thromboembolic events is often underutilised. [7,8] It is estimated that up to 51% of patients eligible for anticoagulant therapy do not receive it. [9] Furthermore, an estimated 86% of patients who suffer from AF and have a subsequent stroke were not receiving adequate anticoagulation therapy following their AF diagnosis. [10]
In contrast, pharmacological treatments for stroke prophylaxis have been associated with an increased risk of intracerebral haemorrhage, particularly amongst the elderly. [11] A study of 170 patients with AF over the age of 85 years demonstrated that the rate of haemorrhagic stroke was 2.5 times higher in those receiving anticoagulant therapy compared to controls (OR=2.5, 95% CI: 1.3-2.7). [12] Therefore, the need to optimise the management of patients with AF in the general practice (GP) setting is of high importance for stroke prevention and requires an individualised pharmacological approach in order to achieve a balance between stroke reduction and bleeding side effects.
Consequently, the development of validated risk stratification tools such as the CHADS2 score (Congestive Heart Failure, Hypertension, Age ≥75 years, Diabetes, Previous Stroke or Trans-ischemic Attack (TIA)) has enabled more accurate identification of AF patients who are at an increased risk of stroke by assessing co-morbidities and additional risk factors to determine the appropriateness of anticoagulation or antiplatelet prophylaxis to reduce the risk of thromboembolic events. [13]
The aim of this research project was to determine the prevalence of AF among patients within a GP cohort and to assess the adequacy of pharmacological stroke prophylaxis according to the CHADS2 criteria. The results of this study will enable GPs to determine whether the current management of patients with AF is adequate and whether closer follow-up of these patients needs to occur in order to minimise associated bleeding and stroke complications.
Methods
Study design and ethics
This study was a retrospective cohort study of the prevalence, patient characteristics and adequacy of anticoagulation according to the CHADS2 score in GP patients with AF over a 3-year period. The study was approved by the University of Wollongong Human Research Ethics Committee (Appendix 1, HREC 13/031).
Participants
Participants were identified using a search of the practice database (Best Practice, Version 1.8.3.602, Pyefinch Software Pty Ltd), at a South Coast NSW Medical Centre using the database search tool. Search criteria included any patient (recorded as alive or deceased) who attended the practice with a recorded diagnosis of AF over a 3-year period (between November 2010 – November 2013) and were ≥50 years of age. This included both patients with long-term AF diagnosed before the study period in addition to those newly diagnosed with AF during the study period. The total number of all patients aged ≥50 years who attended the practice at least once during the same period was recorded to determine the prevalence of AF at the practice.
Exclusion Criteria
Exclusion criteria included patients <50 years of age, patients with incomplete medical records or those diagnosed with AF who subsequently moved from the practice during the study period.
CHADS2 score
The CHADS2 score was chosen for the purpose of this study as it is a validated risk-stratification tool for patients with AF. [13-15] The scoring system assigns one point each for the presence of Congestive Heart Failure, Hypertension, Age ≥75 years or Diabetes and assigns two points if a patient has a history of previous Stroke or TIA. AF patients with a CHADS2 score of 0 are considered to be at low risk of a thromboembolic event (0.5 – 1.7% per year stroke rate); a score of 1 indicates intermediate risk (2.0% per year stroke rate) and a score ≥2 indicates high risk (4.0% per year stroke rate). [16]
Data Search and Extraction
Patient data was manually extracted from individual patient records, coded and recorded into a spreadsheet (Microsoft Excel, 2007). Basic data including date of birth and sex were recorded. Date of AF diagnosis (assessed as the first documented episode of AF within the patient record) and co-morbidities including hypertension, congestive heart failure, diabetes, stroke or TIA were included if documented within the patient medical record. Correspondence from specialists and hospital discharge summaries were also analysed for any diagnosis made outside of the medical centre and not subsequently recorded in the medical record.
Lifestyle factors were recorded from the practice database including
alcohol use (light/moderate/heavy or none) and smoking status (nonsmoker, ex-smoker or current smoker). Complications arising from
pharmacological prophylaxis (including any documented bleeding or
side-effects) or discontinuation of treatments were included. Individual
patient visits were analysed for any documented non-compliance with
medications. Where possible, cause of death was also recorded.
Adequacy of Anticoagulation
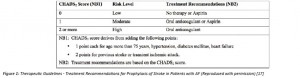
Individual CHADS2 scores were determined for each patient at baseline,
12 months and 3 years. At each of these time points, CHADS2 scores
were compared to each patient’s medication regime (i.e. no medication
use, an anticoagulant agent or an antiplatelet agent). The use of other
medications for the treatment of AF (for example, agents for rate or
rhythm control) was not assessed. Patients were then classified as
being undertreated, adequately treated or over-treated according to
the CHADS2 score obtained at baseline, 12 months and 3 years as per
the current therapeutic guidelines (Figure 1). [17]
Adequate treatment was considered to be patients receiving treatments
in accordance with the therapeutic guidelines. [17] Undertreated
patients included those who received no treatment when an oral
anticoagulant was indicated (CHADS2 score ≥2). Over-treated patients
included those treated with an oral anticoagulant where it was not
indicated according to the current guidelines (CHADS2 score = 0).
Statistical Analysis
Results are presented as mean ± standard deviation. A p-value of <0.05 was considered to be statistically significant. One-way ANOVA was used to assess between-group differences in CHADS2 scores at each time point (Baseline, 12 months and 3 years). Descriptive data is presented where relevant. Prevalence of AF at the practice was calculated using the formula; (patients with AF ≥50 years / total number of patients ≥50 years at the practice, X 100).
Results
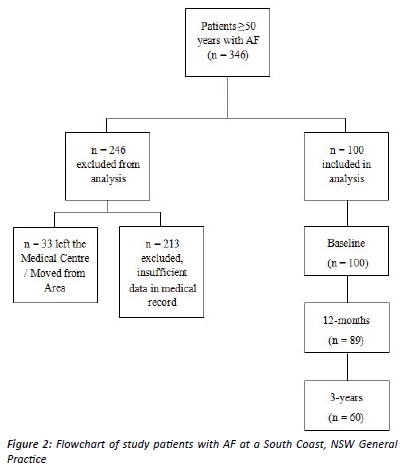
A total of 346 patients with AF aged ≥50 years were identified. Of these, 246 participants were excluded – (n=213 due to insufficient data within their medical record, and n=33 patients had left the practice during the study period) leaving a total of 100 patients for inclusion in the analysis (Figure 2). Due to the nature of the search strategy (which identified any patient with AF during the period of November 2010-November 2013), both newly-diagnosed patients and patients with long-term AF were included in the analysis. Therefore, long-term data was available for n=89 participants at 12 months, and n=60 participants at 3 years. There were no statistically significant differences in age (p=0.91) or sex (p=0.86) between the included and excluded participants.
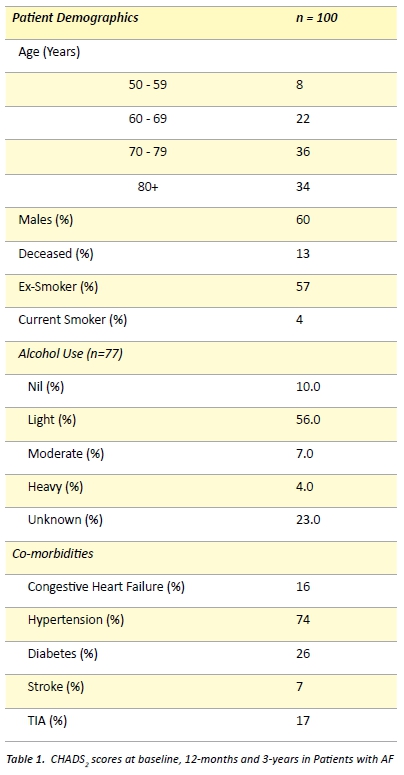
Including all patients initially identified with AF (n=346), the overall prevalence of AF among patients at the practice was 5.8%. Participant characteristics are presented in Table 1. The mean age of participants at diagnosis was 74.9 ± 10.0 years, with more males suffering from AF (60%) compared to females (40%). Over half of patients had a history of smoking (57%), and hypertension was the most common co- morbidity (74%). 13% of participants were listed within the practice database as being deceased.
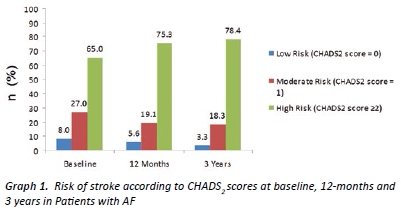
At baseline, 65.0% of patients were classified as high risk of stroke (CHADS score ≥2). This increased to 75.3% of patients and 78.4% of patients at 12 months and 3 years, respectively (Graph 1). There were no patients with a CHADS2 score of 6 at any of the study time points. Analysis of participants who had 3-year follow-up data available (n=60) demonstrated a statistically significant increase in average CHADS2 scores among patients between baseline vs. 12 months (p<0.05) and baseline vs. 3 years (p<0.01). There was no statistically significant difference in CHADS2 scores between 12 months vs. 3 years (p=0.54).
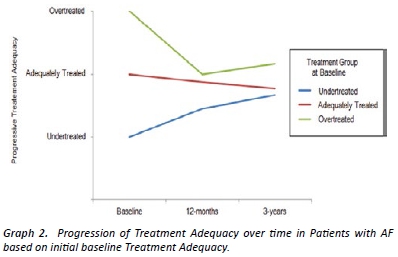
Graph 2 demonstrates changes in treatment adequacy over time based on patients’ initial treatment group allocation at baseline. For patients who were initially identified as being undertreated at baseline, there was a trend toward adequate treatment by 3-years. For patients initially identified as over-treated at baseline, the trend towards adequate treatment occurred more rapidly (p=non-significant) (on average by 12 months).
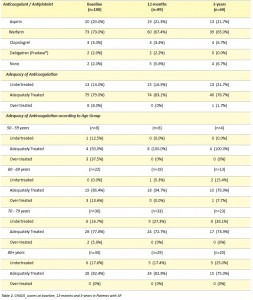
Patient pharmacological treatments and adequacy of treatment at baseline, 12 months and 3 years are shown in Table 2.
There were several reported side-effects and documented instances of medication cessation from anticoagulation and antiplatelet therapy. A total of eight patients were non-compliant and ceased warfarin during the study period and eight patients had their warfarin ceased by their treating doctor (reason for cessation unknown). A further eight patients ceased warfarin therapy due to side-effects (Intracranial haemorrhage (n=1), Gastrointestinal bleeding (n=3), Haematuria (n=1), Unknown bleeding (n=3)). One patient ceased aspirin due to oesophageal irritation. No other pharmacological therapies were ceased due to side-effects. Warfarin was ceased in one case due to an elective surgical procedure.
A total of two patients suffered an embolic or haemorrhagic stroke and a further two patients suffered a TIA during the study period. Prior to their thromboembolic event, one patient was undertreated with aspirin (CHADS2 score = 2), one was adequately treated with clopidogrel (CHADS2 score = 1) and a further one patient was undertreated on aspirin (CHADS2 score = 3). Cause of death was unknown in six patients. No patients had stroke or TIA listed as their cause of death in their medical record.
Discussion
It has been suggested that Australian patients with AF may not be receiving optimal prophylactic anticoagulant and antiplatelet medications for the prevention of thromboembolic events. [7,8] The aims of this retrospective cohort study were to assess stroke risk and the adequacy of anticoagulation in 100 AF patients ≥50 years over a 3 year period in a GP setting.
Results from the current study indicate that overall, the use of anticoagulant and antiplatelet strategies for stroke prophylaxis was appropriate in the majority of cases and consistent with published therapeutic guidelines. [17] The prevalence of AF at the practice of 5.8% was similar with other studies, which report a prevalence of AF in the GP setting of between 4-8%. [18, 19] In the current study, there were more males with AF than females, however this trend has also been found in several other studies which have reported a higher prevalence of AF amongst males. [15,18]
CHADS2 scores increased between baseline and 12 months and baseline and 3 years. This increase was to be expected as patients are likely to gain additional risk factors as they age. The majority of patients at all time points were at high risk of stroke (CHADS2 score ≥2), with warfarin or similar anticoagulation therapy being indicated.
Overall, treatment adequacy increased between baseline and 12 months (79% versus 83.1%), then decreased by 3 years (83.1% versus 76.7%). This trend is likely to represent aggressive management of AF at the initial diagnosis then a decline in optimal stroke prophylaxis as patients age, develop additional side-effects or become at increased risk of falls. Additionally, older patient groups (those >70 years) were more likely to be undertreated. This may be due to several factors, including patient non-compliance with warfarin therapy, doctor reluctance to prescribe warfarin to patients at risk of falls, and the incidence of side-effects such as bleeding. Similar causes of under- treatment of elderly patients with AF have been outlined in other studies. [20,21] In younger patients, there was a trend towards over- treatment at the time of diagnosis.
In the current study, one patient suffered an embolic stroke during the study period and two patients had a TIA. Appropriately, all three of these patients were subsequently changed to warfarin. One patient who was adequately treated on warfarin with a CHADS2 score of 1 was changed to aspirin following an intracranial haemorrhage (and consequently remained classified as adequately treated). Although these were isolated cases within the study, it should be noted that the life-long morbidity of stroke for these individuals is significant.
Strengths of the current study include the large number of patients and the comprehensive assessment of medical records for the main study outcomes of CHADS2 scores and anticoagulation or antiplatelet therapies. By assessing individual medical records, a comprehensive assessment of patient data was available for inclusion in the study analysis.
There are some limitations in the current study. As data was extracted from an existing database of patient medical records (which was not kept for the purpose of conducting research) there were some instances of missing or incomplete data. However, the majority of missing data was, in general, relating to the patient’s social history (such as smoking rates and alcohol use), which were not central to the main research aims and would not have influenced the results.
A thorough assessment of medication regimes was able to be carried out for the purpose of this study. As all medication changes are automatically recorded by the Best Practice program at each visit, the author is confident that this aspect of the data is accurate. However, it should be noted that it is possible that some patients may have been taking over the counter aspirin, which may not have been recorded on their medication list and consequently some patients may have been assessed as ‘undertreated’. An additional consideration relates to the use of warfarin and whether patients’ prescribed warfarin were within the therapeutic range, however, the assessment of multiple INR readings for each patient over a 3-year period was thought to be beyond the scope of this study. Only two patients at the practice had been prescribed NOACs (Dabigatran) for anticoagulation, therefore analysis of this medication was limited.
The calculation of CHADS2 scores was able to be assessed for all patients. Although most co-morbidities were well documented, theremay have been some limitations with regards to the identification of some co-morbidities such as hypertension, diabetes and the presence of congestive heart failure among some patients. For example, in some instances some patients did not have a recorded diagnosis of hypertension, but a review of blood pressure readings demonstrated several high systolic blood pressure readings which could have been diagnostic for hypertension. Where this occurred, patients were not considered to have hypertension or congestive heart failure and were not assigned an additional CHADS2 point.
The CHADS2 score was chosen for the purpose of this study due to its simplicity and validation for the identification of patients at risk of stroke [13-15]. More recently, refinements to the CHADS2 score has led to the development of the CHA2DS2-VASC score, which assigns additional points to higher age groups, female patients and patients with vascular disease. [22] The CHA2DS2-VASC score provides a more comprehensive overview of stroke risk factors in an individual and has also been validated for the purpose of determining the need for pharmacological stroke prophylaxis. More recently, studies have shown that application of the CHA2DS2-VASC score is most useful for clarifying the stratification of patients within the low-intermediate stroke risk categories (i.e. determining those with CHADS2 scores of 0-1 who are truly at low risk and do not require aspirin). [23] Because the aims of the current study were to identify patients at high risk of stroke and determine the appropriateness of their treatment, the CHA2DS2-VASC score was not utilised in this study. However, it should be noted that the CHA2DS2-VASC may provide additional clarification in the assessment of patients with low-intermediate CHADS2 scores.
An additional consideration in this study relates to the nature of the AF suffered by patients. Although patients were included if they had a known diagnosis of AF, it is almost impossible to determine how long patients had already been suffering from AF prior to and after their diagnosis. In addition, it was not possible to determine whether patients had paroxysmal or sustained/chronic AF. However, it has been demonstrated that there may be little difference in outcomes for patients with paroxysmal versus persistent AF, [24,25] with a large cohort study comparing stroke rates in patients with paroxysmal versus sustained AF reporting no significant difference in rates of stroke (3.2% versus 3.3%, respectively). [24] Therefore, it is unlikely that determination of paroxysmal and sustained AF patterns would have influenced results of the current study.
Conclusion
The results obtained from this study will allow GPs to optimise the management of patients with AF in the community setting. Although this study found that the management of patients with AF at the practice is consistent with the current guidelines in the majority of cases, further improvements can be made to minimise the risk of stroke among patients with AF, especially with regards to targeting undertreated patients. Additionally, the current study may raise greater awareness of the incidence of AF within the practice and the need to assess stroke risk and treat patients accordingly, especially as CHADS2 scores were rarely recorded formally at the time of diagnosis. GPs are well placed to optimise the treatment of AF and prevent strokes though treatment of co-morbidities and implementing lifestyle interventions, such as encouraging smoking cessation and the minimisation of alcohol use, and may further reduce the incidence of stroke and TIA in patients with AF.
Acknowledgements
The author would like to acknowledge Dr Darryl McAndrew, Dr Brett Thomson, Prof Peter McLennan, Dr Judy Mullan and Dr Sal Sanzone for their contribution to this research project.
Conflict of interest
None declared.
Correspondence
S Macleod: dm953@uowmail.edu.au
References
[1] Furberg, C, Psaty, B, Manolio, T, Gardin, J, Smith, V, Rautaharju, P. Prevalence of atrial fibrillation in elderly subjects (The Cardiovascular Health Study). Am J Cardiol. 1994; 74 (3): 236-241.
[2] Wong, C, Brooks, A, Leong, D, Roberts, K, Sanders, P. The increasing burden of atrial fibrillation compared with heart failure and myocardial infarction: A 15-year study of all hospitalizations in Australia. Arch Int Med. 2012; 172 (9): 739-741.
[3] Lip, G, Boos, C. Antithrombotic treatment in atrial fibrillation. Heart. 2006; 92 (2): 155-161.
[4] Medi, C, Hankey, G, Freedman, S. Stroke risk and antithrombotic strategies in atrial fibrillation. Stroke. 2010; 41: 2705-2713.
[5] Gould, P, Power, J, Broughton, A, Kaye, D. Review of the current management of atrial fibrillaiton. Exp Opin Pharmacother. 2003; 4 (11): 1889-1899.
[6] Brieger, D, Curnow, J, Anticoagulation: A GP primer on the new anticoagulants. Aust Fam Physician 2014, 43 (5): 254-259.
[7] Gladstone, D, Bui, E, Fang, J, Laupacis, A, Lindsay, P, Tu, J, et. al. Potentially preventable strokes in high-risk patients with atrial fibrillation who are not adequately anticoagulated. Stroke. 2009; 40: 235-240.
[8] Olgilvie, I, Newton, N, Welner, S, Cowell, W, Lip, G. Underuse of oral anticoagulants in atrial fibrillation: A systematic review. Am J Med. 2010; 123 (7): 638-645.
[9] Pisters, R, Van Oostenbrugger, R, Knottnerus, I. The likelihood of decreasing strokes in atrial fibrillation patients by strict application of guidelines. Europace. 2010; 12: 779-784. [10] Leyden, J, Kleinig, T, Newbury, J, Castles, S, Cranefield, J, Anderson, C, et. al. Adelaide Stroke Incidence Study: Declining stroke rates but many preventable cardioembolic strokes. Stroke. 2013; 44: 1226-1231.
[11] Vitry, A, Roughead, E, Ramsay, E, Preiss, A, Ryan, P, Pilbert, A, et. al. Major bleeding risk associated with warfarin and co-medications in the elderly population. Pharmacoepidem Drug Safe. 2011; 20 (10): 1057-1063.
[12] Fang, M, Change, Y, Hylek, E, Rosand, J, Greenberg, S, Go, A, et. al. Advanced age, anticoagulation intensity, and risk for intracranial hemorrhage among patients taking warfarin for atrial fibrillation. Ann Int Med. 2004; 141: 745-752.
[13] Gage B, Waterman, A, Shannon, W. Validation of clinical classification schemes for predicting stroke: Results from the National Registry of Atrial Fibrillation. JAMA. 2001; 285: 2864-2870.
[14] Khoo, C, Lip, G. Initiation and persistance on warfarin or aspirin as thromboprophylaxis in chronic atrial fibrillation in general practice. Thromb Haemost. 2008; 6: 1622-1624.
[15] Rietbrock, S, Heeley, E, Plumb, J, Van Staa, T. Chronic atrial fibrillation: Incidence, prevalence, and prediction of stroke using the congestive heart failure, hypertension, age >75, diabetes mellitus, and prior stroke or transient ischemic attack (CHADS2) risk stratification scheme. Am Heart J. 2008; 156: 57-64.
[16] UpToDate. Antithrombotic therapy to prevent embolization in atrial fibrillation. [Internet]. 2013 [Cited 2014 Mar 9]. Available from: http://www.uptodate.com/contents/antithrombotic-therapy-to-prevent-embolization-in-atrial-fibrillation
[17] e-Therapeutic Guidelines. Prophylaxis of stroke in patients with atrial fibrillation.[Internet]. 2012 [Cited 2014 Mar 9]. Available from: http://etg.hcn.com.au/desktop/index.htm?acc=36422
[18] Fahridin, S, Charles, J, Miller, G. Atrial fibrillation in Australian general practice. Aust Fam Physician. 2007; 36.
[19] Lowres, N, Freedman, S, Redfern, J, McLachlan, A, Krass, I, Bennet, A, et. al. Screening education and recognition in community pharmacies of atrial fibrillation to prevent stroke in and ambulant population aged ≥65 years (SEARCH-AF Stroke Prevention Study): A cross-sectional study protocol. BMJ. 2012; 2 (Online).
[20] Hobbs, R, Leach, I. Challenges of stroke prevention in patients with atrial fibrillation in clinical practice. Q J Med. 2011; 104: 739-746.
[21] Hickey, K. Anticoagulation management in clinical practice: Preventing stroke in patients with atrial fibrillation. Heart Lung. 2012; 41: 146-156.
[22] van Starr, T, Setakis, E, Ditanna, G, Lane, D, Lip, G. A comparison of risk stratification schemes for stroke in 79,884 atrial fibrillation patients in general practice. Thromb Haemost. 2011; 9: 39-48.
[23] Lip, G. Atrial fibrillation and stroke prevention: Brief observations on the last decade. Expert Rev Cardiovasc Ther. 2014; 12 (4): 403-406.
[24] Hart, R, Pearce, L, Rothbart, R, McAnulty, J, Asinger, R, Halperin, J. Stroke with intermittent atrial fibrillation: Incidence and predictors during aspirin therapy. J Am Coll Cardiol. 2000; 35: 183-187.
[25] Nattel, S, Opie, L. Controversies in atrial fibrillation. Lancet. 2006; 367: 262-272.