How do the specialty choices and rural intentions of medical students from Bond University (a full-fee paying, undergraduate-level medical program) compare with other (Commonwealth Supported Places) Australian medical students?
Edward Teo, Kathleen Lockhart, Jennifer Pushparajah, David Waynforth, Janie Smith
Tuesday, September 1st, 2015
Introduction: Australian medical schools are demonstrating an
increased interest in full-fee paying education, which warrants
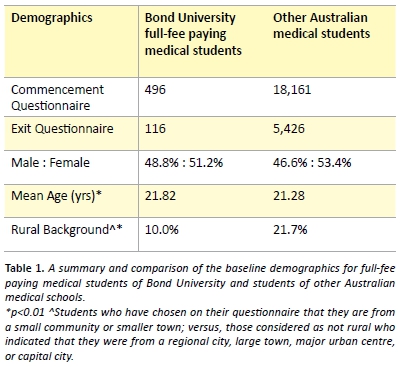
assessment of possible ramifications on the profile of the Australian medical workforce. This study aims to identify differences in demographics, specialty preferences and rural intentions between domestic full-fee paying undergraduate medical students and all other (CSP) Australian medical students. Methods: The data of 19,827 medical students was accessed from the Medical Schools Outcomes Database from 2004-2011. This was then analysed using logistic regression and McNemar’s test to identify differences in specialty choice and preferred location of practice. Results: Demographically, full-fee paying medical students of Bond University and other Australian medical students were similar in age and gender. However, Bond medical students were less likely to come from a rural background (10% versus 21.7%) and, even after performing logistic regression analysis, still showed
a greater preference for future urban practice at both entry and
exit of medical school than all other students (entry questionnaire OR = 3.3, p < 0.01, and exit questionnaire OR = 3.9, p < 0.05). There was no significant difference in preference for higher-paid medical specialties or those in short-supply between Bond medical students and all other Australian medical students.Conclusion: Full-fee paying medical students of Bond University demonstrate similar future specialty preferences but are far more likely to come
from an urban background and choose urban over rural practice than other medical students. Further research is necessary to better understand the implications of full-fee paying education on the medical workforce.

Introduction
Australian medical schools are demonstrating an increased interest in providing full-fee paying education; in 2004 there were 160 places for domestic full-fee paying Australian medical students (1.6% of all students), which increased to 932 (7%) by 2008 and 871 (5.1%) in 2013. [1,2] This trend warrants the assessment of possible ramifications on the profile of the Australian medical workforce in terms of specialty and geographical distribution. [3]
There are a number of medical student characteristics and experiences that are known to guide medical training and ultimately impact on the nature and location of their specialty choices. [4-8] This includes demographic characteristics such as gender, background (rural or urban origin), personal and family factors (whether a student has a partner or children), education, personality and interests. [9] Previous research has indicated a pattern of gender distribution amongst medical specialties, where women are more likely to choose general practice and men are more likely to enter other specialist careers (such as surgery, which remains a very male-dominated field). [9] Similarly, male doctors tend to place a higher emphasis on financial remuneration and women are generally more concerned about working hours and flexibility of practice. [8] The perceived prestige and lifestyle factors associated with certain specialties plays a significant role in specialisation choice. [8,10-12] Clinical exposure to specialty fields is key in influencing some of these preconceived views. [10,13]
It is well documented that there is a significant shortage and maldistribution of doctors in remote and rural Australia, reflecting an increasing awareness that this inadequacy of healthcare needs to be addressed in these communities. [5,6,8-10,12,14-19] Only 23% of Australian doctors practise in places of significant workforce need, where the number of doctors per head of population is 54-65% of that in metropolitan areas. [16] Although programs, research and government incentives have been introduced over the past 20 years to address these problems, the Rural Doctors Association of Australia has reported that less than 5% of medical school graduates have taken up rural practice in the last 15 years and the majority of doctors working in rural areas are international medical graduates on restricted provider numbers. [12,19,20]
Among the many factors that influence medical students to take up rural practice after graduation, the strongest indicator is a rural background, closely followed by positive rural placements. [5,9,15,16,20,21] Rural-practicing doctors are two to four times more likely to be of rural background than those practising in urban areas. [5] However, between 34% – 67% of rural doctors originate from urban backgrounds which is attributed in part to students’ rural clinical exposure through scholarships and placements such as the John Flynn Placement Program and the Rural Undergraduate Support and Coordination (RUSC) funded rural experience. [5,22] Training opportunities such as Rural Clinical Schools are also effective in influencing students towards a rural career by allowing students to experience the benefits of rural life first-hand whilst providing effective and innovative medical education. [7,22,23] Now many programs are available for medical students that offer exposure to rural practice. [6,12,17,23,24]
Bond University was the first institution to offer a full-fee paying undergraduate medical course in Australia in 2005 [25], with no direct funding from the Australian Government. Several well-established medical schools followed suit by introducing up to 50% more full- fee paying places in their current medical programs to cater for the student surplus, including international students. [26] While fees vary amongst medical schools for both domestic and international full-fee paying places, they are generally between of $30,000 to $60,000 per annum for a four to six year education. [27] Domestic full-fee paying students do have the option of accessing loans under the Government ‘Fee-Help’ program to cover a portion of their tuition fees; they are entitled to a lifetime maximum of $112,134 for a medical education (as of 2013) with 20% simple interest, repayable upon graduation and employment. [27]
The aim of this study was to determine whether full-fee paying Australian medical students differ significantly from other medical students in terms of future intended specialty career and rural/urban location of practice. This level of financial burden has raised significant concerns about its implications of medical education accessibility and future workforce specialty distribution. We hypothesised that full-fee paying students would indicate an increased preference for pursuing future urban practice and higher-paying specialties.
Methods
Data was provided by the Medical Schools Outcomes Database (MSOD), a project of the Medical Deans Australia and New Zealand association that is funded by Health Workforce Australia as a means of evaluating rural medical education initiatives. [19] Commencement of Medical School Questionnaires (CMSQ) and Exit Questionnaires (EQ) are administered to all medical students on entry to and graduation from all Australian medical schools and at the end of the first postgraduate year.
Independent variables
The main independent binary variable of comparison represented whether the student attended Bond University’s full-fee paying undergraduate medical program or not. Other independent variables included in each analysis were the student’s sex, age when they began medical school, the year they began medical school, whether they are of rural background and their marital status.
Dependent variables
Preference for urban versus rural future medical practice was re- categorised into a binary variable from the original questionnaire categories: Those who chose to practice in a small community, small town, regional city or town were considered to be rural candidates. Those who chose to practice in a capital or major city centre were considered to be urban candidates.
Two variables were created to explore preferences for future medical specialty. The first of the two is a binary variable that assesses the preference for choosing a higher-paying specialty. Students who chose surgery, obstetrics and gynaecology, radiology, intensive care medicine or emergency medicine—which are the top five specialties rated as the highest paid in the ‘2010 Medicine in Australia: Balancing Employment and Life (MABEL)’ study—were considered in pursuit of a higher-paying specialty. The second binary variable examined the preference for choosing a specialty in-demand (not necessarily highest paid). [24] Students who chose general practice, psychiatry, obstetrics and gynaecology, pathology, ophthalmology or radiology—which are predicted to be the top six specialties in short supply by 2025 by the Health Workforce of Australia (HWA)—were considered in pursuit of a specialty in-demand. [28]
Statistical analysis
Independent samples t-tests were used to compare differences between medical students of Bond University and all other Australian medical students on demographic background variables (Table 1). Logistic regression was used for comparisons between full-fee paying medical students of Bond University and all other Australian medical students in analyses of preferences for the three dependent variables listed above. Data on preferences for rural versus urban practice, for the top five paid, and six most in-need specialties were analysed at two data collection time points: on entry to medical school (CMSQ) and exit from medical school (EQ), resulting in six logistic regression models comparing full-fee paying undergraduate medical students with all other medical students. McNemar’s test was used to analyse changes in student rural future practice and specialty preferences between the time that they entered and exited medical school, and logistic regression to explore changes through time between cohorts in these preferences.
Ethics Approval
Approval was provided by all universities for the MSOD project, which applies to this paper. Permission was requested and approval given by MSOD to use their data for this research article (MR-2013-002).
Results
The results of the McNemar’s tests showed no statistically significant difference for full-fee paying medical students of Bond University who completed both entry and exit questionnaires (n = 94), but that in all other medical students (n = 3760) there was a significant drop in intention to practice rurally, and an increase in preference for a top 5 paid specialty and specialties predicted to be in short supply (p-values < 0.001). In addition, there was evidence of cohort effects in CMSQ preferences amongst all medical students: between 2005 and 2011 cohorts entering medical school, later cohorts of students had a greater preference for urban future practice. The cohort effect odds ratio was 1.07 (p < 0.001; 95% CI: 1.04-1.10). Later cohorts were less likely to select a future specialty on the list of six most in-need (OR = 0.95, 95% CI: 0.94-0.98, p < 0.001) but were not more or less likely to prefer a top 5 paid specialty. No significant cohort effects were observed in the exit questionnaire analyses, although it should be noted that the exit data only included four cohorts (2008-11).
Both commencement and exit of medical school surveys showed that full-fee paying medical students of Bond University had a significantly greater preference for future urban practice than other Australian medical students (Figure 1).
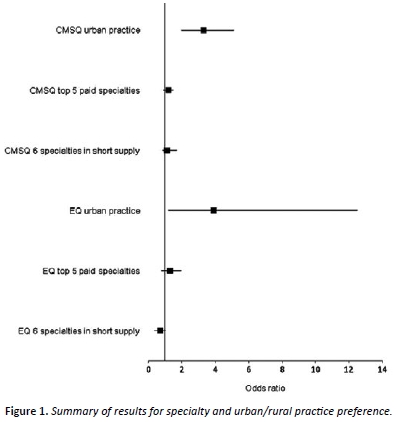
Age on entry to medical school, gender, marital status and whether the student was from a rural background were statistically controlled in all six analyses.
Analyses performed using logistic regression; 95% CIs aforementioned in Results text; p < 0.05.
OR > 1.0 indicates variable in favor of full-fee paying medical students of Bond University.
OR < 1.0 indicates variable in favor of other Australian medical students.
Analyses shows that full-fee paying medical students of Bond University were neither more likely to have a preference for the top five paid medical specialties, nor more likely to pursue the top 6 specialties predicted to be in need by 2025, when compared with all other medical students in Australia (Table 2).
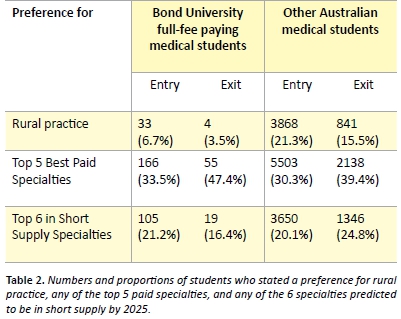
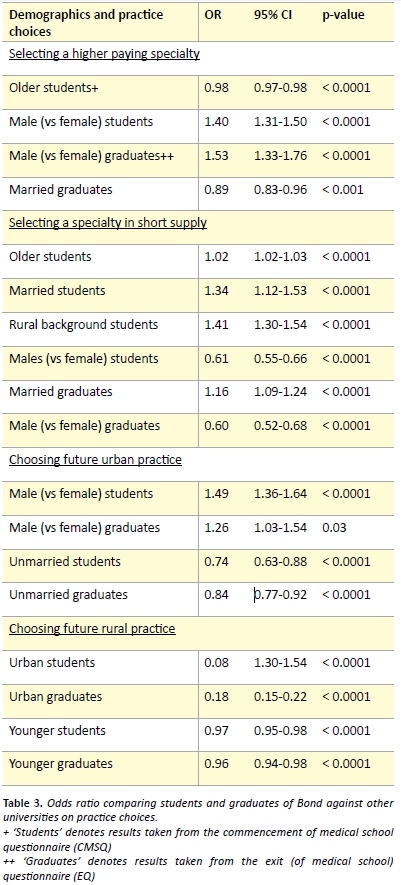
Of the variables which were statistically controlled in the logistic regression analyses, a number were significant predictors of the three outcomes. These findings have been summarised in Table 3. At entry to medical school, older students and women were less likely to select a top five paid specialty and women remained less likely to select a top five paid specialty at exit. Married students were significantly less likely to choose any top five paid specialty as their first preference on exit. Specialties in short supply were selected at entry by those who were older, married, from a rural background or female and at exit by those who were married or female. Coming from an urban background was a strong predictor of not preferring future rural medical practice at both entry and exit from medical school and men were oriented towards urban practice. Younger students stated less preference for rural practice and unmarried students stated a lesser preference for future urban practice.
Discussion
Interestingly, in contrast to our hypothesis, we found that full-fee paying medical students of Bond University were not more or less likely to prefer the highest-paid medical specialties when compared with other Australian medical students. There were also no significant differences in preference for specialties predicted to be in short supply. This result implies that the full-fee paying nature of education is not a significant influential factor in future specialty preferences whilst supporting the idea that this choice may be guided by other demographic and experiential factors documented in the literature.
More students in general (that is, including students of Bond and all other medical schools) had a tendency to select a top-paid specialty by the end of medical school compared to entry.
So the potential generalised ‘commercialisation’ of students’ motivations during medical training remains a point of concern despite the apparent validation of full-fee paying training as an unlikely implicating factor. There are no papers in the current Australian literature specifically exploring the factors influencing medical students in this choice, so we can only theorise on the circumstances affecting the decisions to pursue a higher-paid specialty. This trend may indicate that students begin medical school with more altruistic and rural intentions, but change their minds during training and come to place greater importance on financial return as they mature through their educational experience. Cohort effects may also play a role (that is, whether more recent student cohorts are more oriented towards future urban practice and career earnings). The trends of student specialty preference being affected by financial debt obtained during training and potential remuneration in higher paid specialties are being increasingly explored in American and Canadian literature. [29, 30]
At exit from medical school, fewer Australian medical students, in general, planned to work in a rural area than at entry, despite the numerous incentives and rural programs to encourage rural medical practice. The decrease in preference for rural practice by graduation in all Australian medical students may reflect the small number of regional medical schools or limited opportunity for rural placements, and factors such as specialty choice and training in urban areas. It is nonetheless clear that full-fee paying Bond medical students are more likely to prefer urban practice when compared against other Australian medical students. This may suggest the need for further modification of medical school recruitment and admission processes at privately funded institutions to focus on students who demonstrate either a rural background or interest in rural practice. There are current opportunities for students who are keen to undertake rural clinical clerkships at all medical schools through various in-curricular and extra- curricular activities. However, unlike their commonwealth-supported counterparts, privately-funded medical schools are not mandated to enforce their students to receive this rural exposure. Ensuring a rural clinical rotation could be a potential avenue for encouraging more students to pursue rural and remote practice. James Cook University (JCU) has designed its medical program specifically to recruit and prepare doctors to work in rural and remote locations. Their program is characterised by a selection process targeting students of regional and remote backgrounds, a rural community orientated curriculum, increased engagement with Aboriginal and Torres Strait Islander health issues and more frequent and extended rural clinical placements. [31] As a result, at graduation, 88% of JCU medical students intend to practise outside Australian capital cities, compared to 31% of graduates from other medical schools. [31]
The conclusions of this study are limited by the difference in sample size between full-fee paying undergraduate medical students and all other students (496 compared to 18161). This restricted the potential for statistically significant subgroup data analysis. A further qualitative study would be useful in clarifying student motivations and influencing factors in decision making of future specialty choice and location of practice. There is, as yet, no long-term data of how students’ preferences translate to actuality, with the first students who contributed to the MSOD project still in their early postgraduate years. Ongoing follow-up of students may also shed further light on factors that influence doctors at all stages of training. There is an increasing emphasis on medical schools becoming ‘socially accountable’ in their training of physicians, in order to respond to current and future health needs and challenges in society, which includes the maldistribution of doctors. [32] The initiatives that medical schools undertake in an effort to fulfil the criteria presented by the World Health Organisation (WHO) for social accountability are designed to impact the training of medical students and therefore may be partially accountable for graduate specialty preferences. Further research is being conducted to clarify whether a full-fee-paying medical student education and potential associated debts can influence specialty choice, particularly higher income specialties. [33]
Conclusion
Full-fee paying medical students of Bond University are more likely to come from an urban background and prefer urban over rural practice at exit of medical school when compared with all other Australian medical students. This is a point of concern and may inform future modifications to medical school admission processes as well as more opportunities for rural clinical exposure in the curriculum. Nonetheless, they remain similar to all other Australian medical students in terms of demographic characteristics and preference for higher-paying specialties and those in short supply. Future research is directed to assess the long term impact on medical workforce distribution and specialty choice of full-fee paying medical education in Australia.
Acknowledgements
The research on which this paper is based used data provided by the Medical Schools Outcomes Database (MSOD) Project, Medical Deans Australia and New Zealand. We are grateful to the Australian Government Department of Health and Ageing for funding the project from 2004 – 2011, to Health Workforce Australia for funding from 2011 onwards and to the medical students and graduated doctors who participated.
Conflict of interest
None declared.
Correspondence
E Teo: eteo@outlook.com
References
[1] Jolly, R. Briefing report: Medical practitioners education and training in Australia. Parliamentary Library (Australia). 2009. Available from: http://apo.org.au/node/17809
[2] Australian Government Department of Health. Medical training review panel: Seventeenth report. 2014. Available from: http://www.health.gov.au/internet/main/ publishing.nsf/Content/work-pubs-mtrp
[3] Australian Medical Students’ Association. Concerning increase in private medical places Australian Medical Students’ Association [Internet]. 2010 [cited 2014 Aug 29]. Available from: https://www.amsa.org.au/press-release/20100607-concerning-increase-in-private- medical-places/
[4] Laurence C, Elliott T. When, what and how South Australian pre-registration junior medical officers’ career choices are made. Medical Education. 2007;41(5):467-75.
[5] Tollhurst HM, Adams J, Stewart SM. An exploration of when urban background medical students become interested in rural practice. Rural Remote Health. 2006;6:452.
[6] Eley DS, Synnott R, Baker PG. A decade of Australian rural clinical school graduates: Where are they and why? Rural Remote Health. 2012;12:1937.
[7] Pearson SA, Rofle I, Clare R. A comparison of practice outcomes of graduates from traditional and non-traditional medical schools in Australia. Medical Education. 2002;36:985-91.
[8] Thistlethwaite JE, Leeder SR, Kidd MR. Addressing general practice workforce shortages: Policy options. Med J Aust. 2008;189(2):118-21.
[9] Ward AM, Kamien M, Lopez DG. Medical career choice and practice location: Early factors predicting course completion, career choice and practice location. Medical Education. 2004;38:239-48.
[10] Creed PA, Searle J, Rogers ME. Medical specialty prestige and lifestyle preferences for medical students. Social Sciences and Medicine. 2010;71(1084-1088).
[11] Tolhurst H, Stewart M. Becoming a GP: a qualitative study of the career interests of medical students. Aust Fam Physician. 2005;34(3):204-6.
[12] Krahe LM, McColl AR, Pallant JF. A multi-university study of which factors medical students consider when deciding to attend a rural clinical school in Australia. Rural Remote Health. 2010;10:1477.
[13] Spencer RJ, Cardin AJ, Ranmuthugala G, Somers GT, Solarsh B. Influences of medical students’ decisions to study at a rural clinical school. Aust J Rural Health. 2008;16(5):262-8.
[14] Eley D, Young L, Ptzybeck TR. Exploring temperament and character traits in medical students: A new approach to increase a rural workforce. Medical Teaching. 2009;31:79-84.
[15] Adams ME, Dolland J, J H. Development of a questionnaire measuring student attitudes to working and living in rural areas. Rural Remote Health. 2005;5:327.
[16] Critchley J, DeWitt DE, Khan MA. A required rural health module increases students’ interest in rural health careers. Rural Remote Health. 2007;7(688).
[17] Denz-Penhey H, Murdoch JC. Reported reasons of medical students for choosing a clinical longitudinal integrated clerkship in an Australian rural clinical school. Rural Remote Health. 2009;9:1093.
[18] Humphreys JS, Prideaux D, Beilby JJ. From medical school to medical practice: A national tracking system to underpin planning for a sustainable medical workforce in Australasia. Med J Aust. 2009;191(5):244-5.
[19] Jones M, Humphreys J, Prideaux D. Predicting medical students’ intentions to take up rural practice after graduation. Medical Education. 2009;43:1001-9.
[20] Jones M, Humphreys JS, McGrail MR. Why does a rural background make medical students more likely to intend to work in rural areas and how consistent is the effect? A study of the rural background effect. Aust J Rural Health. 2012;20:29-34.
[21] Playford DE, Evans SF, Atkinson DN. Impact of the Rural Clinical School of Western Australia on work location of medical graduates. Med J Aust. 2014;200:104-7.
[22] Australian Government Department of Health. Rural Clinical Schools Program. 2014. Available from: http://www.health.gov.au/clinicalschools
[23] Couper I, Worley PS, Strasser R. Rural longitudinal integrated clerkships: lessons from two programs on different continents. Rural Remote Health. 2011;11:1665.
[24] Cheng TC. What factors influence the earnings of general practitioners and medical specialists? Evidence from the medicine in Australia: Balancing employment and life survey. Health Econ. 2012;21(11):1.
[25] Prideaux D. Medical education in Australia: Much has changed but what remains? Medical Teacher. 2009;31(2):96-100.
[26] Hubraq H. CMSQ National Data Report. Canberra, ACT: Medical Deans Australia and New Zealand, Inc; 2011.
[27] Information for Commonwealth Supported Students and HECS-HELP. In: EaWR DoE, editor. Canberra, ACT: Commonwealth of Australia; 2012.
[28] Australian Government. Health Workforce Australia (HWA) Report 2025 for Doctors, Nurses and Midwives. Health Workforce Australia. 2012 [cited 2014 Aug 29]; Available from: https://www.hwa.gov.au/sites/uploads/HW2025_V3_FinalReport20121109.pdf.
[29] Morra DJ, Regehr G, Ginsburg S. Medical students, money, and career selection: Students’ perception of financial factors and remuneration in family medicine. Fam Med. 2009;41(2):105-10.
[30] Rosenblatt R, Andrilla C. The impact of U.S. medical students’ debt on their choice of primary care careers: An analysis of data from the 2002 medical school graduationq uestionnaire. Acad Med. 2005;80(9):815-19.
[31] Sen Gupta T, Murray, R, Hays R, Woolley T. James Cook University MBBS graduate intentions and intern destinations: A comparative study with other Queensland and Australian medical schools. Rural and Remote Health. 2013;13(2313).
[32] Larkins SL, Preston R, Matte MC, Lindemann IC, Samson R, Tandinco FD. Measuring social accountability in health professional education: Development and international pilot testing of an evaluation framework. Med Teach. 2013;35(1):32-45.
[33] Hays R, Lockhart K, Teo E, Smith J, Waynforth D. Full medical program fees and medical student career intention. Med J Aust. Pending Publication.
