The impaired student: Substance abuse in medical students
Lewis Fry
Tuesday, December 1st, 2015
Substance use disorder has been a significant issue within the medical profession throughout history. It is recognised as an important issue of concern, particularly due to its associated mortality, morbidity and social consequences. Although a substantial body of literature addresses this issue amongst doctors, there is little discussion focusing on medical students. This review summarises the existing literature available on the epidemiology, common presenting features, management, legal implications and mandatory notification requirements of substance abuse in the medical student. Limited evidence suggests concerning levels of hazardous alcohol use exists in medical students, however alcohol and drug use is not comparatively higher than the general student population. While early detection is optimal for harm prevention, signs and symptoms of substance abuse are subtle and easily missed. Prevention and early intervention is critical, and it is important for students to recognise possible signs of substance abuse in their colleagues, as the biggest barrier to treatment is denial. Once detected, current evidence from Physician Health Programs suggests a service to manage the student’s multidisciplinary care, follow up and return to study obtains the best outcome. As a chronic medical condition that carries significant risk of harm to the impaired student – and potentially to patients – all health professionals should be aware of this issue and their mandatory reporting obligations.
Substance use disorder (SUD) amongst doctors is an issue of significant concern. It is estimated the lifetime prevalence of substance abuse in Australian doctors is approximately 8%. [1] There is limited literature or discussion, however, addressing this issue in the context of the most junior members of the profession, medical students. The university experience is often coupled with alcohol use and occasionally with casual illicit drug use, but this is, to some extent, accepted, perhaps as part of youthful exuberance, experimentation or a rite of passage. [2] For some, however, this substance use may manifest as, or progress to, substance abuse: a pattern of drug or alcohol use that is detrimental both to the individual and to society. [3] For the substance-abusing medical student, there is a wide scope for serious implications personally, professionally and with the public.
This article aims to highlight the importance of this topic and provide information on the concept of substance use disorder, common signs of substance abuse, management, reporting requirements and legal implications. It also addresses why it is imperative there is awareness for this issue in medical students to prevent serious health consequences and risk to the public.
Terms within this article
Substance use disorder or substance abuse: A chronic condition characterised by a pathological pattern of behaviours related to substance use, manifesting as two or more symptoms of: impaired control of drug use; social impairment at work, school or home; risky use; tolerance or withdrawal. [4]
Substance dependence: An inability to control substance use, despite problems caused by use. [5] This may manifest physically or psychologically with tolerance or withdrawal. Dependence and drug abuse are not separate entities within the Diagnostic and Statistical Manual 5 (DSM-5), however these terms are prevalent in the cited literature.
Impairment: A physical or mental impairment, disability, condition or disorder (including substance abuse or dependence) that detrimentally affects, or is likely to detrimentally affect, a practitioner’s capacity to practise the profession. [6]
How common is student substance abuse?
There is little recent, comprehensive data on student substance abuse, with most studies occurring in the 1980s-1990s and concerning rates of use rather than abuse. [5] Furthermore, prevalence studies are hindered by surveys requiring self-reporting of abuse and varied case definitions. With these limitations, the available data on student substance use is summarised below.
Alcohol use and abuse
Use of alcohol in the general student population is common, with consumption occurring in approximately 96% of Australians aged 18-21 years. For medical students in particular, international studies have indicated that rates of lifetime alcohol usage range between 62.3% and 98.1%. [2,5,7-11] Male medical students have higher levels of intake compared to females and hazardous alcohol use is significantly higher in those with high levels of psychological distress. [12] The BeyondBlue study of medical students and doctors found concerning rates of moderate-risk (21%) and high-risk (4%) drinking amongst medical students in Australia. [12] Moderate risk is classed as a hazardous intake level and high risk is associated with harmful drinking patterns, as assessed by the World Health Organisation Alcohol Use Disorders Identification Test (AUDIT). [12] This level of drinking, however, appears low in comparison to the general university population, which has an approximately 8.1% rate of harmful drinking. [12,13]
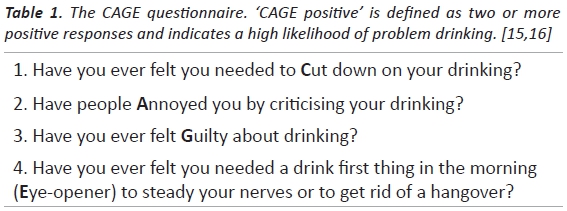
Internationally, 50% of medical students in the UK consumed above the recommended amount. [8] Using the CAGE questionnaire (Table 1), 22.4% of junior Turkish medical students and 52.5% of Irish medical students were found to be CAGE positive. [10,11] Of medical students who drink, 60.5% of men and 72.2% of women engaged in binge drinking, with 36.8% of men and 58.2% of women suggesting that their performance had been affected at least one day in the past month by alcohol consumption. [8] While the BeyondBlue study noted that drinking levels decreased with age, other data suggests that as students progress through their clinical years and beyond, a greater number of students drink, and drink more heavily. [10,14]
Drug use
Rates of illicit substance abuse in medical students appear comparable to, or less than that of, the general population, with data falling between 3-10%. [17] BeyondBlue reports show low rates, with 10.2% of students engaged in illicit drug use 2-3 times a month, and 0.5% 1-6 times a week. [12]
Drugs of abuse may be recreational, for example cannabis or stimulants, or prescription, such as benzodiazepines, opiates or propofol. Amongst junior students, the most common drug of abuse is cannabis and is often likely to be the first used before medical school. [2,8,14] Other illicit or prescription drugs are less common, however alcohol and cannabis might be considered gateway drugs to these. In one study, those who used cannabis were more likely to be drinking heavily than non-users and those who used illicit drugs had also used cannabis. [14] It is reported that medical students are increasingly being offered illicit drugs, and more are accepting them. [11] Abuse of illicit drugs, such as cocaine, or prescription drugs, such as benzodiazepines, was more likely to occur once at university. [2]
Notably, as students progress to become doctors, patterns of drug abuse change with increasing rates of prescription drug abuse. [5,10] Drugs of choice vary by medical specialty as to what is easiest to obtain; for example, anaesthetists have high rates of propofol and opiate abuse, whereas other specialties such as psychiatrists are more likely to abuse benzodiazepines. [1,18,19].
Recognition of substance abuse
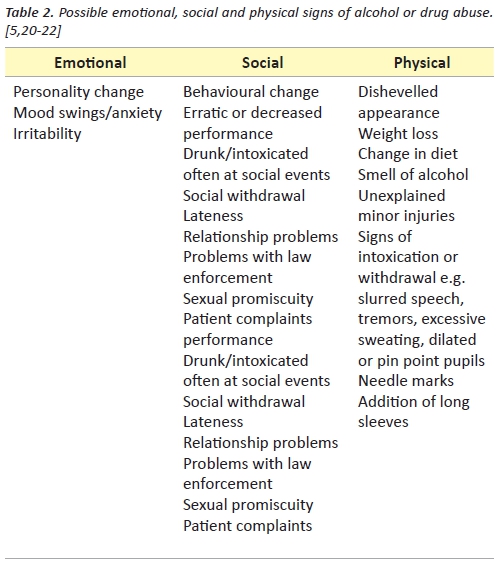
Signs of substance abuse are both subtle and varied, and can be easily missed. They are often disguised by the affected practitioner. Denial is common, and often it is the person with the disorder that is last to acknowledge a problem. [20] Early detection can prevent the development of significant harm. Table 2 lists possible emotional, social and physical signs of alcohol or drug abuse.
Reporting requirements
The impaired physician is a concept defined under national law as a physical or mental impairment, disability, condition or disorder (including substance abuse or dependence) that detrimentally affects, or is likely to detrimentally affect, a practitioner’s capacity to practise the profession. [6] For a student, the impairment must detrimentally affect, or be likely to detrimentally affect, the student’s capacity to undertake clinical training. This means impairment is defined by a student’s reduced capacity to learn, a quite broad definition. For a notification to the Australian Health Practitioner Regulation Agency (AHPRA) to be made, however, there must be a belief that their impairment could cause public harm, for instance intoxication at work. [6,23]
Two forms of notification can be made to AHPRA. [6] Mandatory notifications compel practitioners or education providers to make a notification if they form a reasonable belief that a student has an impairment that may place the public at substantial risk of harm in the course of their clinical training, or are practising whilst intoxicated with alcohol or drugs. Voluntary notifications about a student can be made by anyone if they form a reasonable belief that a student has an impairment that may cause public harm.
Consequences of notification may include the suspension of a student’s registration, the imposition of conditions of practice, further health assessment, and possible long-term impacts on their ability to continue their studies and future registration (depending on expert advice in each case). [6,23] For students, it is important to recognise the possible future career consequences of alcohol or drug abuse.
Management of the impaired student
Treatment of impairment is both complex and individualised and there is no standard protocol for treating impaired medical students. Treatment may be managed by the student and their treating team, or may be arranged by AHPRA or the medical board as a result of a notification. Individual medical school impairment policies likely vary and are not reviewed here. A majority of reviewed American school policies require direct referrals for management of suspected substance abuse cases, and one third forego disciplinary treatment for those impaired students who self-refer to promote seeking early intervention. [5] Depending on the substance(s) involved, treatment may include features such as inpatient treatment and detoxification, 12 step programs or use of therapeutic agents (e.g. naltrexone). [3]
Referral to a long-term support program with a specific focus on doctors’ health is optimal. Within Australia, available services and models of support vary from state to state. Most states offer a Doctor’s Health Advisory Service telephone counselling service, with support offered by experienced practitioners. [24] The Victorian Doctors’ Health Program (VDHP) offers the only full-time physician health program (PHP) of its kind in Australia. It is confidential, independent of AHPRA and open to both doctors and medical students. [25] PHPs were pioneered in the United States to assist in the rehabilitation of impaired physicians. They do not directly provide treatment but provide evaluation and diagnosis, facilitation of formal addiction treatment, on-going confidential support, case management, biochemical and workplace monitoring, and return-to-work support as required on a case-by-case basis. [25,26] A core component is an individualised care contract lasting up to five years to ensure compliance with the appropriate treatment plan devised. This may include a case manager, psychiatrist, addiction specialist, psychologist, general practitioner or social worker. Ongoing peer support is also recommended through a facilitated Caduceus collegial support group open to medical practitioners and students with substance abuse issues, and has been shown to play an important role in recovery. [1] The VDHP offers three types of programs of different levels of support, ranging from intensive case management to wellbeing and support programs and long term follow up, depending on what is required in each case and the phase of recovery. These programs are successful, with studies consistently demonstrating success rates of 75-90% after five years for American physicians treated through PHPs. [27,28] Preliminary data from the VDHP program indicates similar Australian five-year success rates. [25]
The evidence-based success of these programs suggests that similar services should be available for all doctors. However, cost is a significant issue. The average American state PHP costs USD$521,000 annually to manage between 65 to 75 physicians per year, primarily paid for by an additional $23 charge to licensing fees, whilst formal treatment costs are covered by health insurance and personal physician contributions. [27] It is important to note that some PHPs produce better outcomes than others and that implementation should replicate published successful models and be followed with outcome evaluations. [29,30]
Further to specific services available to doctors, there is a wealth of support available through the pastoral support and wellbeing services of universities that can be accessed in a student capacity. One proactive university even developed and successfully implemented an Aid for the Impaired Medical Student program to oversee medical student recovery management, although little has been published on this recently. [31]
Fighting the “conspiracy of silence”
Boisaubin and Levine discuss the concept of a “conspiracy of silence” where the impaired physician, his/her colleagues, friends and family have a tendency to dismiss their suspicions and suppress their concerns, with a belief that the physician is fine, or capable of solving his/her issues. [32] They state “denial is the most consistent hallmark of this disease process, for both colleagues and the susceptible physician.” This is a key barrier to treatment, and only increases with professional advancement in a medical culture of not admitting weakness, let alone acknowledging the presence of a medical condition laden with stigma. Participants in the VDHP substance use programs were most likely to have been referred by colleagues, employers or treating doctors, compared to self-referral or referral from regulatory bodies. [1] This demonstrates the importance of students and educators being aware of the signs of substance abuse in others, and knowing the options available to assist.
Future implications
There is little data about the risks of student substance abuse, but death or near fatal overdose is the presenting symptom in 7-18% of doctors. [33] Alarmingly, recent data demonstrates anaesthetists abusing propofol have a 45% mortality rate. [19] Substance abuse is also often coupled with psychiatric morbidity and stress-related disorders. Harm to patients is a real risk, either indirectly through impairment of capacity and decision making, or directly, such as in the well-publicised case of the fentanyl-abusing doctor spreading Hepatitis C to women undergoing pregnancy terminations. [34]
There is no clear longitudinal data to demonstrate whether substance abuse as a student is associated with substance abuse as a doctor. This article does not enter the debate as to whether impairment due to substance abuse as a student should preclude a student pursuing a career intimately associated with a range of drugs of abuse, such as opiates. Without prescribing rights, students are more limited in their access to the wide range of substances, compared with their qualified colleagues. It was noted that, of those surveyed in an evaluation of the VDHP Caduceus program, substance abuse issues began in medical school for 16% of the respondents. [1] Furthermore, the diagnosis of alcohol abuse is commonly delayed, often for years, and can start with patterns of high risk drinking.
Conclusion
In conclusion, substance use disorder has enormous impacts, including health issues, patient risk, mandatory notification requirements, future career implications and ultimately escalation to more dangerous substances. It is a chronic medical condition and management requires a multidisciplinary team, long-term support, sensitivity and experience. It is important to recognise that, while medical students are often high functioning and high achieving and generally appear to have similar rates of substance use to the general university population, they are not immune to substance abuse issues. In a profession with high levels of psychological distress, burnout and minor psychiatric morbidity, it is necessary to have a higher index of suspicion. [12] The biggest barrier to treatment is denial, not only by the impaired student, but also by friends, family and colleagues. It would therefore seem imperative that student substance abuse is detected early and treatment provided immediately to prevent the serious consequences of ignoring the situation.
If this article raises concerns for you or anyone you know, information on your local state service can be accessed at the Australasian Doctors’ Health Network website http://www.adhn.org.au/. Crisis support is available 24hrs/day from Lifeline Australia on 13 11 14.
For useful general wellbeing information focused on medical students, Keeping Your Grass Greener is a fantastic guide available from the Australian Medical Student Association at: https://www.amsa.org.au/ initiatives/community-and-wellbeing/keeping-your-grass-greener/
Acknowledgements
The author wishes to acknowledge Dr Kym Jenkins, Clinical Director of the Victorian Doctor’s Health Program for information on the management of substance abuse in Australia.
Conflict of interest
None declared.
Correspondence
L Fry: lefry3@student.monash.edu
References
[1] Wile C, Jenkins K. The value of a support group for medical professionals with substance use disorders. Australas Psychiatry [Internet]. 2013;21(5):481–5. Available from: http://apy.sagepub.com/lookup/doi/10.1177/1039856213498289
[2] Baldwin DC, Hughes PH, Conard SE, Storr CL, Sheehan DV. Substance Use Among Senior Medical Students: A Survey of 23 Medical Schools. JAMA. American Medical Association; 1991;265(16):2074–8.
[3] American Society of Anesthesiologists Chemical Dependency Task Force. Model Curriculum on Drug Abuse and Addiction for Residents in Anesthesiology [Internet]. 2002 [cited 2015 Jan 11]. pp. 1–23. Available from: http://uthscsa.edu/gme/documents/ModelCurriculumonDrugAbuseandAdditionforResidentsinAnesthesiology.pdf
[4] American Psychiatric Association. Substance-Related and Addictive Disorders. Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition. American Psychiatric Association; 2014.
[5] Dumitrascu CI, Mannes PZ, Gamble LJ, Selzer JA. Substance Use Among Physicians and Medical Students. Medical Student Research Journal [Internet]. 2014;3:26–35. Available from: http://msrj.chm.msu.edu/wp-content/uploads/2014/04/MSRJ-Winter-2014-Substance-Use-Among-Physicians-and-Medical-Students.pdf
[6] Australian Health Practitioner Regulation Agency (AHPRA). Legal Practice Note – Students with an Impairment – LPN 5 [Internet]. AHPRA. 2013 [cited 2015 Jan 16]. pp. 1–4. Available from: http://www.ahpra.gov.au/Publications/legal-practice-notes.aspx
[7] Victorian Drug and Alcohol Prevention Council. 2009 Victorian Youth Alcohol and Drug Survey [Internet]. Department of Health (VIC); 2010. pp. 1–92. Available from: http://www.health.vic.gov.au/vdapc/downloads/vyads-report-01092010.pdf
[8] Pickard M, Bates L, Dorian M, Greig H, Saint D. Alcohol and drug use in second-year medical students at the University of Leeds. Med Educ. 2000;34(2):148–50.
[9] Conard S, Hughes P, Baldwin DC, Achenbach KE, Sheehan DV. Substance use by fourth- year students at 13 U.S. medical schools. J Med Educ. 1988;63(10):747–58.
[10] Akvardar Y, Demiral Y, Ergor G, Ergor A. Substance use among medical students and physicians in a medical school in Turkey. Soc Psychiatry Psychiatr Epidemiol. Steinkopff-Verlag; 2004;39(6):502–6.
[11] Boland M, Fitzpatrick P, Scallan E, Daly L, Herity B, Horgan J, et al. Trends in medical student use of tobacco, alcohol and drugs in an Irish university, 1973–2002. Drug Alcohol Depend. 2006;85(2):123–8.
[12] BeyondBlue. National Mental Health Survey of Doctors and Medical Students. 2014 Aug 22:1–156.
[13] Said D, Kypri K, Bowman J. Risk factors for mental disorder among university students in Australia: findings from a web-based cross-sectional survey. Soc Psychiatry Psychiatr Epidemiol. 2012;48(6):935–44.
[14] Newbury-Birch D, Walshaw D, Kamali F. Drink and drugs: from medical students to doctors. Drug Alcohol Depend. 2001;64(3):265–70.
[15] Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry. 1974;131(10):1121–3.
[16] Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA. 1984;252(14):1905–7.
[17] Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: causes, consequences, and proposed solutions. Mayo Clin Proc. 2005;80(12):1613–22.
[18] Hughes PH, Storr CL, Brandenburg NA, Baldwin DC Jr., Anthony JC, Sheehan DV. Physician Substance Use by Medical Specialty. J Addict Dis. 2008;18(2):23–37.
[19] Fry RA, Fry LE, Castanelli DJ. A retrospective survey of substance abuse in anaesthetists in Australia and New Zealand from 2004 to 2013. Anaesth Intensive Care. 2015;43(1):111–7.
[20] Bryson EO, Silverstein JH. Addiction and Substance Abuse in Anesthesiology. Anesthesiology. 2008;109(5):905–17.
[21] The Association of Anaesthetists of Great Britain and Ireland. Drug and Alcohol Abuse amongst Anaesthetists Guidance on Identification and Management [Internet]. The Association of Anaesthetists of Great Britain and Ireland. 2011 [cited 2015 Jan 5]. 1–40. Available from: http://www.aagbi.org/sites/default/files/drug_and_alcohol_abuse_2011_0.pdf
[22] Berge KH, Seppala MD, Schipper AM. Chemical dependency and the physician. Mayo Clin Proc. 2009;84(7):625–31.
[23] Australian Health Practitioner Regulation Agency (AHPRA). Legal Practice Note – Practitioners and Students with an Impairment – LPN 12 [Internet]. AHPRA. 2012 [cited 2015 Apr 14]. Available from: http://www.ahpra.gov.au/documents/default.aspx?record=WD13%2f9983&dbid=AP&chksum=cNb7VU68ZOvtXoQiaFacKA%3d%3d
[24] Doctors Health Advisory Service. Australasian Doctor’s Health Network [Internet].Australasian Doctors Health Network. 2015 [cited 2015 Apr 14]. Available from: http://www.adhn.org.au/
[25] Wile C, Frei M, Jenkins K. Doctors and medical students case managed by an Australian Doctors Health Program: characteristics and outcomes. Australas Psychiatry. 2011;19(3):202–5.
[26] DuPont RL, McLellan AT, Carr G, Gendel M, Skipper GE. How are addicted physicians treated? A national survey of Physician Health Programs. J Subst Abuse Treat. 2009;37(1):1–7.
[27] McLellan AT, Skipper GS, Campbell M, DuPont RL. Five year outcomes in a cohort study of physicians treated for substance use disorders in the United States. BMJ. 2008;337:a2038.
[28] Skipper GE, Campbell MD, DuPont RL. Anesthesiologists with Substance Use Disorders: A 5-Year Outcome Study from 16 State Physician Health Programs. Anesth Analg. 2009;109(3):891–6.
[29] DuPont RL, Skipper GE. Six Lessons from State Physician Health Programs to Promote Long-Term Recovery. J Psychoactive Drugs. 2012;44(1):72–8.
[30] Oreskovich MR, Caldeiro RM. Anesthesiologists recovering from chemical dependency: can they safely return to the operating room? Mayo Clin Proc. 2009;84(7):576–80.
[31] Ackerman TF, Wall HP. A programme for treating chemically dependent medical students. Med Educ. 1994;28(1):40–6–discussion55–7.
[32] Boisaubin EV, Levine RE. Identifying and assisting the impaired physician. Am J Med Sci. 2001;322(1):31–6.
[33] Garcia-Guasch R, Roigé J, Padrós J. Substance abuse in anaesthetists. Curr Opin Anaesthesiol. 2012 Apr;25(2):204–9.
[34] Petrie A. Abortion doctor knew he had hepatitis C, court told [Internet]. The Age. 2011 [cited 2015 Mar 10]. Available from: http://www.theage.com.au/victoria/abortion-doctor-knew-he-had-hepatitis-c-court-told-20111206-1oh80.html